INTRODUCTION
A spinal cord injury (SCI) typically results in loss of function, which can include both mobility disabilities and sensory impairment. The severity of the injury is influenced by its location and the amount of spinal tissue damage; as such SCI can results in either partial or complete paralysis while affecting body systems that affect respiration1. Respiratory problems are also experienced by athletes who use wheelchairs, including those with SCIs or other disabilities, which can affect their sports ability, general wellness, and overall standard of living. Tetraplegia, for example, is associated with loss of function or complete paralysis of the diaphragm muscles, i.e. the main respiratory muscle, resulting in reduced lung capacity2.
Athletes with SCI are often subject to weakness of the intercostal and abdominal muscles, which reduces their capacity to take deep breaths and cough effectively. Furthermore, those who use wheelchairs in sport typically have reduced vital capacity and lung volume after deep inhalation, due to restricted chest mobility caused by muscle dysfunction. Indeed, SCI has been demonstrated to decrease total lung capacity, especially in cases characterised by high injury levels3.
Wheelchair athletes are often more susceptible to respiratory infections, such as pneumonia, as the respiratory muscles can impair the coughing ability needed for effective removal of airway secretions4. Severe SCI also reduces the efficiency of oxygen exchange in the lungs by disrupting the matching of ventilation and perfusion5. In addition, the risk of respiratory infections can be further increased by impaired immune system function6.
During physical activity, wheelchair athletes may also experience exercise-induced bronchoconstriction7. Due to their restricted lung volume and weakened respiratory muscles, wheelchair athletes experience reduced oxygen delivery when engaging in propulsion and sprint activities, increasing physical exhaustion. They are also more prone to accelerated respiratory muscle fatigue than able-bodied athletes during intense and extended periods of exercise: when the demand for oxygen rises suddenly, the compromised respiratory muscles are pushed to their limits much earlier. Hence, to compete successfully in paralympic competitions, wheelchair athletes need to build robust respiratory strength to allow them to propel their chairs while improving endurance and athletic performance8.
The strength of the diaphragm and respiratory muscles can be improved through Respiratory Muscle Training (RMT) programs, which aim to improve both lung function and breathing capability. RMT may be delivered using several device types. Pressure-threshold types use a spring-loaded valve that only opens when the user generates a preset inspiratory pressure; these devices are simple, provide a consistent load independent of flow, and are widely used in clinical trials9. Various RMT programmes have been trialled in athletes with SCI, though the number remains limited. For example, West et al.10 conducted an inspiratory muscle training programme in wheelchair rugby athletes with cervical SCI using a pressure-threshold device; the findings indicate significant increases in maximal inspiratory pressure (MIP) and improved respiratory endurance. However, recent studies focused on wheelchair athletes remain scarce due to the problems associated with reduced lung volume and coughing, and respiratory muscle weakness caused by SCI. As such, despite extensive evidence documenting their respiratory challenges, there remains a lack of targeted research on RMT interventions in athletes with spinal cord injury11,12.
These respiratory problems negatively influence both the athletic performance and the overall health of wheelchair athletes. While RMT programmes have achieved favourable outcomes among non-athletes with chronic respiratory diseases, research on their influence on pulmonary function and endurance remains limited in wheelchair athletes13.
The use of RMT devices, such as pressure-threshold, flow-resistive, isocapnic hyperpnea, and incentive spirometry apparatus, represents a new treatment modality for enhancing both lung performance and sports agility in wheelchair athletes. The aim of the study was to examine the effects of a RMT program on pulmonary function and endurance in wheelchair athletes with SCI.
MATERIALS AND METHODS
Ethical considerations
All investigations gained Institutional ethics committee approval (LPU/IEC-LPU/2025/1/43). Clinical trial registry no CTRI/2025/02/081360. Every participant provided written consent for participation and maintained the right to resign from the study at their convenience, with no adverse consequences.
Study Design
This study employed a pre–post intervention design conducted over four weeks. Assessments were carried out at baseline (pre-intervention) and after the intervention period (post-intervention). Athletes were allocated into an intervention group receiving the RMT program or to a control group; the measurements focused on pulmonary function and endurance performance.
Participants
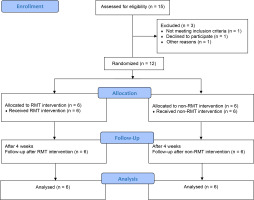
The participant recruitment, allocation, follow-up and analysis stages are presented in a CONSORT flow chart (Figure 1). The athletes were recruited from wheelchair sports training centres associated with Lovely Professional University and from institutions linked to national wheelchair sports federations in Punjab, India. Recruitment was facilitated through professional networks that distributed study invitations and information sheets to competitive wheelchair athletes. Eligible participants were athletes, aged between 25 and 42 years, diagnosed with SCI below the T1 neurological level, engaged in organized wheelchair sports (basketball, rugby, or racing) for at least one year, participating in regular, structured training within recognized sports settings. The athletes were excluded if they had experienced recent cardiorespiratory complications, progressive neurological conditions, history of poor compliance with rehabilitation programs or contraindications to RMT.
As this was a pilot trial, no formal sample size or power calculation was conducted. Feasibility and availability of eligible athletes were the primary considerations for recruitment, with the main aim being to collect preliminary data to inform future, larger-scale studies. The final sample consisted of 12 athletes: wheelchair basketball (n = 5), wheelchair rugby (n = 4), and wheelchair racing (n = 3).
The athletes completed baseline assessments prior to group allocation. Randomization was performed using computer-generated sequences, and allocation was concealed using sealed opaque envelopes. The athletes conducted their training sessions at their respective sports facilities, both indoors and outdoors, as per their usual training schedules.
Data collection
The athletes underwent training sessions in their respective sports, viz. wheelchair basketball, rugby or racing: training frequency five days per week, duration 60–90 minutes per session, and moderate to high intensity, based on perceived exertion or heart rate zone. All athletes performed standardized warm-up exercises before they began the tests.
Propulsion efficiency was measured on a 20-metre indoor flat surface used for standard testing. The athletes were asked to propel the wheelchair at their own comfortable speed over a distance: each test was performed three times, with the efficiency calculated by dividing the mean distance by the number of pushes. Athletes were recommended upper-body exercises that included shoulder and thoracic spine movements, intercostal stretching techniques with three to five diaphragmatic breathing and pursed-lip breathing exercises. The athletes rested for five to seven minutes immediately after the warm-up before starting the specific tests to allow their heart rate and breathing to settle.
To measure endurance, the athletes propelled their wheelchairs as far as possible in twelve minutes on an indoor 20-metre track, the aim being to move as fast as possible sustainably without outside help. The distance covered during the test was recorded as the endurance score. The athletes were asked to propel their wheelchair at a constant submaximal speed; the timer was started when the test began and was stopped when the athlete voluntarily stops due to fatigue or if the heart rate exceeded 85–90% maximum heart rate (HRmax), rate of perceived exertion (RPE) ≥ 17 (very hard). Finally, endurance was calculated as the total duration (in minutes) maintained before stopping. The wheelchair propulsion efficiency test was selected to assess the mechanical efficiency and biomechanical performance of athletes during sport-specific propulsion. Reliability studies in both elite and recreational wheelchair athletes report high intra-class correlation coefficients (ICC > 0.85) for propulsion speed, stroke frequency, and mechanical efficiency14.
The athletes were familiarised with RMT and spirometry in a session a day before baseline testing to improve measurement accuracy and reduce learning effects. The athletes received introductory sessions for the RMT prototype device with pressure gauge and the spirometry equipment. The RMT was prepared especially for the study and was designed to offer resistance to the respiratory muscles during inspiration and expiration using circular tesla valves. The level of breathing resistance for inhaling or exhaling could be set via dials on the machine, ranging from -100 to 200 centimeters of water (cmH₂O), for progressively challenging exercises. This prototype device was calibrated (Standard equipment used: Pressure cum Vacuum Gauge & Differential Pressure Gauge, method: SCP-02 MPV & SCP-04 MPV, Location: at lab Temp: 23 ± 5°C, RH:50 ± 10) under NIIRT- Centre for Calibration, Analysis & Testing (CCR No: C4CAT/2080/C0762).
Briefly, the athletes sat upright and firmly inhaled the air through a flange-style mouthpiece connected to the RMT. The resistance was adjusted to 30 to 50 percent of individual maximal inhaling or exhaling strength, and was increased from low to medium to high resistance each week when rechecked. The athletes from the control group continued their typical routine workouts focusing on strength, wheelchair propulsion practice, practice of skills in their sport, regular aerobic exercise, and standard breathing work15.
Outcome Measures
Pulmonary Function Tests
The following variables were measured using a Helios 401 computerised PFT system (Recorders & Medicare Systems Pvt. Ltd., India) according to American Thoracic Society guidelines21: Forced Vital Capacity (FVC) – litres; Forced Expiratory Volume in 1 second (FEV₁) – litres; FEV₁/FVC ratio – percentage; Peak Expiratory Flow Rate (PEFR) – litres/minute
Respiratory Muscle Strength
Respiratory muscle strength was evaluated based on Maximal Inspiratory Pressure (MIP) and Maximal Expiratory Pressure (MEP) using a respiratory pressure meter. All measurements were taken in a seated position, with a nose clip applied. The athletes performed three maximal attempts, with the highest value recorded.
Sports Performance Assessment
Specific performance-related tests were conducted for each sport: sprint and manoeuvrability tests for wheelchair basketball and rugby athletes, and 100m time trial for wheelchair racing. All performance tests were conducted under supervision for each athlete on their regular training surface.
Intervention Protocols
RMT Protocol
Frequency: five days/week; Duration: 20 minutes/session; Intensity: Initial resistance set at 30% of MIP, progressively increased every week. Exercises: Inspiratory phase: Deep inhalation against resistance; Expiratory phase: forceful exhalation against resistance. Progression: load increased when athletes could perform >15 repetitions without fatigue.
The newly-developed RMT prototype incorporated a spiral Tesla valve, providing resistance during both inspiration and expiration. It featured an adjustable Venturi-type mechanism with three resistance settings: low, medium, and high. The device was calibrated at an NABL-accredited laboratory in Chandigarh, India.
Each participant completed three maximal inspiratory and expiratory efforts, with the highest value recorded for analysis. The athletes remained seated and wore a nose clip during lung function assessment. FVC, FEV1, MIP and MEP were measured using a PFT and pressure gauge device. To avoid physical fatigue, the athletes executed each manoeuvre three times with a minimum 60-second rest period between attempts. The best measurement values (within a 5% tolerance range) from the three successful testing trials were used for the study. Respiratory muscle strength was measured at baseline, and after four weeks of intervention. The collected data was analysed for precision and reliability.
Sports Training Protocol (control group)
Frequency: five sessions/week; Duration: 60–90 minutes/session; Content: Warmup, sport-specific drills, endurance and agility training, followed by cool-down. Environment: Conducted at the official training venue of each athlete under the supervision of their respective sport coaches.
Statistical analysis
The Shapiro–Wilk test was used to assess the normality of the distribution for all outcome variables, viz. FVC, FEV1, MIP, MEP, propulsion efficiency, and endurance. All variables were found to have a normal distribution, but non-parametric tests were used as the sample size was small. Descriptive statistics were prepared to present participant information, i.e. demographic features, initial measurement results, injury conditions and athletic participation background details. In the RMT and control groups, the observed changes in FVC and FEV1 lung function and MIP and MEP respiratory muscle strength, as well as in wheelchair propulsion efficiency and endurance over time, were evaluated using the Mann–Whitney U-test or Wilcoxon signed-rank test. Both injury level (tetraplegia vs. paraplegia) and sport type variation were taken into consideration in the analysis.
RESULTS
The study included 12 participants: eight male and four female (Table 1). The mean age was 32.5 ± 6.2 years, i.e. young to middle age.
Table 1
Characteristics of age, sex and sports type
The standard deviation was small, indicating modest differences in age; this should reduce the confounding impact of age on respiratory muscle strength and athletic performance outcomes. The RMT and control athletes demonstrated similar baseline characteristics and mean ages, indicating a homogeneous adult athlete test sample. The participants were divided into two groups with identical male to female ratios, i.e. four men and two women. Each group contained athletes who participated in wheelchair basketball, wheelchair rugby, and wheelchair racing.
The baseline pulmonary testing results were 80% FVC, 73.3% FEV1, 62.3% MIP and 60.4% MEP in the RMT group, and 77.1% FVC, 70.0% FEV1, 60.5% MIP and 59.8% MEP in the control group. The RMT group demonstrated significant improvements for all measured outcomes (Table 2). The subjects experienced improved pulmonary function over time, with notable increases in FVC (p = 0.012) and FEV₁. Substantial improvements in respiratory muscle strength were found, including MIP and MEP values (p = 0.001). Of the two groups, the RMT group achieved better results for wheelchair propulsion efficiency and endurance time (p = 0.010) after intervention.
Table 2
Non parametric analysis for pre and post-test values of RMT group vs control group
The FVC, FEV1, MIP and MEP results for the RMT and Control groups are given in Figures 2-4. They indicate that both pulmonary capacity (FVC, FEV₁) and strength of the breathing muscles (MIP, MEP) significantly improved in participants who received RMT. These improvements in body functions brought about noticeable advances in propulsion efficiency and endurance; however, no significant change in any outcome was noted for the control group (p > 0.05).
Figure 2
FVC: comparison between RMT and Control groups post-intervention (dark colour – RMT group, and light colour – control group)
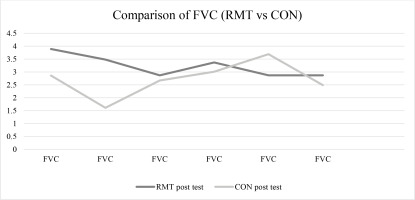
Figure 3
FEV1: comparison between RMT and Control groups post-intervention (dark colour – RMT group, and light colour – control group)
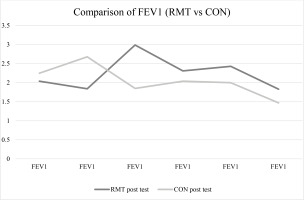
Figure 4
MIP/MEP: comparison between RMT and Control groups post-intervention (dark colour – RMT group, and light colour – control group)
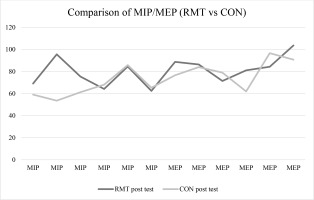
Significant differences were found between the RMT and control groups for several post-intervention variables (Mann–Whitney U-test; Table 3). The RMT group demonstrated significantly higher FVC compared to the control group (U = 28, Z = -2.32, p = 0.023, r = 0.54), with a moderate effect size, and a significant improvement in FEV₁ (U = 21.5, Z = -2.16, p = 0.031, r = 0.44). A substantial increase in inspiratory muscle strength (MIP) was noted in the RMT group (U = 27, Z = -3.82, p = 0.001), with a very large effect size (r = 1.09) as well as in expiratory muscle strength (MEP) (U = 22, Z = -3.41, p = 0.002, r = 0.77), also with a large effect size.
Table 3
Non-parametric test analysis between RMT Group vs Control Group
| Variables | U-value | Z-value | p-value | Effect size (r) |
|---|---|---|---|---|
| FVC (L) | 28 | -2.32 | 0.023* | 0.54 |
| FEV1 (L) | 21.5 | -2.16 | 0.031* | 0.44 |
| MIP (cmH2O) | 27 | -3.82 | 0.001** | 1.09 |
| MEP (cmH2O) | 22 | -3.41 | 0.002** | 0.77 |
| Propulsion Efficiency (%) | 34 | -2.71 | 0.011* | 0.77 |
| Endurance (Minutes) | 28 | -3.15 | 0.004** | 0.73 |
In addition, the RMT group demonstrated significant improvements in propulsion efficiency (U = 34, Z = -2.71, p = 0.011, r = 0.77) and endurance capacity (U = 28, Z = -3.15, p = 0.004, r = 0.73), with large effect sizes.
DISCUSSION
The primary goal of this study was to evaluate the effectiveness of a newly-developed RMT prototype in improving pulmonary function, respiratory muscle strength and sports performance outcomes among athletes with SCI. Our findings indicate that these objectives were achieved, as the participants in the RMT group demonstrated significant improvements across key respiratory and performance-related variables compared to the control group.
A major strength of this study lies in the introduction of a novel, low-cost, and adjustable RMT prototype, which offers dual resistance during inspiration and expiration, distinguishing it from commercially-available devices. It thus provides athletes with a more accessible, yet effective, training tool. Moreover, by highlighting the positive impact of RMT on respiratory health, propulsion efficiency, and endurance, the present study contributes to the growing body of evidence supporting the integration of RMT into sports conditioning and rehabilitation programs for athletes with SCI.
The use of the prototype RMT device was found to improve FVC, FEV₁, MIP, MEP, and endurance in the wheelchair athletes with SCI compared to controls. Hence, respiratory training appears to improve both lung health and sports performance among wheelchair athletes.
The participants in the present pilot study were all paraplegic athletes with a mean age of ~32.5 ± 6.2 years. Our data therefore is representative of an older athletic population than those use in previous studies13,16 characterised by participants with mean ages ranging from 15 to 40 years. This distinction is important, as age may influence respiratory muscle strength and training responsiveness. The current study included both male and female participants with SCI, but sex distribution was not a key determinant of the outcomes, nor was it central to the study objectives. Therefore, this discussion focuses on the effect of RMT on overall improvements in respiratory muscle strength and functional capacity in this population, irrespective of sex distribution.17
The participant sample was composed of 41.7% wheelchair basketball athletes, 33.3% wheelchair rugby players and 25.0% wheelchair racing athletes. In contrast, Lomax et al.20 focused on endurance-trained athletes. Also, Nunes Júnior et al.16 tested wheelchair rugby players, who based their training on endurance; in these athletes, RMT achieved sport-related adaptations i.e. better lung results. Wheelchair rugby is a contact sport with high-intensity, that demands repeated sprints, changes in direction, and explosive upper body movements17,18.
Previous research by HajGhanbari et al.13 on individuals with SCI indicates that respiratory muscle strength training (RMST) can enhance inspiratory muscle strength, expiratory flow, and overall aerobic capacity in populations with respiratory limitations. The authors also report significant improvements in MIP and peak expiratory flow following RMST. Similarly, Soumyashree and Kaur19 report that targeted inspiratory training improved respiratory efficiency and aerobic performance in athletes. These findings are relevant to the present study, as they support the rationale that strengthening the respiratory musculature can improve both pulmonary function and performance-related outcomes. Our study develops on this by confirming that a novel RMT prototype achieves similar benefits specifically in athletes with SCI. Our outcomes have moderate and high effect sizes (from 0.44 to 1.09): spirometric measures like FEV₁ and MIP often have less room for improvement in healthy or trained individuals, as noted previously13,19.
The significant improvements observed in respiratory muscle strength, lung function, propulsion efficiency and endurance highlight the potential benefits of the RMT program. Rather than focusing on statistical details, these findings emphasize the practical value of incorporating RMT into training protocols for athletes with SCI. Such improvements not only contribute to enhanced respiratory health but also have direct implications for athletic performance by increasing efficiency and endurance. Our findings support the role of a structured RMT program as a clinically-meaningful and functionally-relevant intervention that may be integrated alongside conventional training approaches.
Previous studies in individuals with SCI have demonstrated that RMT can improve ventilatory capacity and exercise tolerance by significantly enhancing inspiratory and expiratory pressures; the tested RMT programme improved inspiratory muscle strength (20-30%) and peak expiratory flow (PEF) (15%), and decreased perceived exertion among paraplegics20. A similar improvement was noted in the current study although FVC was used as the primary outcome instead of PEF.
Although studies involving able-bodied athletes cannot be directly compared with our population, they provide useful benchmarks for understanding the magnitude of respiratory adaptations18. Liaw et al. reported that people with paraplegia who underwent inspiratory muscle training (IMT) demonstrated a 35% increase in MIP, highlighting the effectiveness of targeted respiratory interventions in this population. In comparison, a 22% mean improvement (14 cmH₂O) in MIP was observed among participants using the RMT prototype in the present study. While the two studies achieved different degrees of improvement, both achieved positive outcomes; this reinforces the clinical relevance of respiratory training in individuals with SCI. Importantly, the gains observed in our trial suggest that even a novel, lowcost RMT device can improve inspiratory muscle strength, which may translate into improved respiratory health and functional performance in wheelchair athletes 15.
Sports such as wheelchair basketball, and wheelchair rugby require repeated high-intensity bursts of activity, where enhanced inspiratory and expiratory pressures can improve ventilatory efficiency and delay fatigue. Endurance-based wheelchair racing places substantial demands on respiratory and cardiovascular systems, and improved propulsion efficiency and respiratory endurance may contribute to prolonged performance and reduced perceived exertion. Our findings indicate significant increases in volume-based pulmonary function measures (FVC and FEV₁) and in pressure-based respiratory muscle strength parameters (MIP and MEP) following RMT. The MIP and MEP values reflect the strength of the diaphragm, intercostal and abdominal muscles. Our findings demonstrate that changes in MIP values (in this case, from 62 to 76 cmH2O) can indicate a significant change in respiratory muscle strength. They also indicate that the RMT group demonstrated enhanced endurance, as noted in previous studies reporting improved aerobic performance in athletes with SCI; in these cases, RMT training was found to support breathing, enabling better oxygen availability for active muscles during wheelchair propulsion, thereby delaying fatigue20. The assessment of propulsion efficiency in the present study research provides original results about its positive impact on wheelchair propulsion mechanics21.
Our present findings therefore suggest that the benefits of RMT are not confined to sport-specific outcomes, but also extend to functional autonomy and long-term health maintenance for athletes with SCI in their everyday lives. Improved respiratory function has considerable relevance for daily life in individuals with SCI who rely on a wheelchair for both sport and everyday mobility. Enhancements in inspiratory and expiratory muscle strength not only support better performance during training and competition but also improve overall respiratory health and reduce the risk of pulmonary complications; they also increase tolerance for daily physical activities such as transfers, propulsion, and community mobility14. Previous research has emphasized that stronger respiratory muscles promote independence and quality of life21 by facilitating greater endurance and efficiency in wheelchair propulsion.
Unlike many commercially-available devices, which are often designed for the general population without considering the functional limitations of individuals with SCI, our prototype offers adjustable resistance, low cost and ease of integration into training routines. The device could support broader interventions aimed at improving cardiovascular fitness, reducing respiratory complications, and promoting independence in daily life for individuals with SCI.
The tested RMT programme based on our prototype has practical applications for both enhancing sports performance and improving general respiratory health, daily functionality, and independence in athletes with SCI. These results support the inclusion of RMT in multidisciplinary training and rehabilitation programs, offering coaches, physiologists, and physiotherapists a cost-effective and evidence-based tool to maximize both performance and quality-of-life outcomes.
LIMITATIONS
The data were acquired from a small sample size. This was determined by both the feasibility of the studied sports and the availability of suitable wheelchair athletes; however, the main goal was to collect preliminary data to help guide future studies. In addition, not all physical activity levels were controlled. Also, the intervention was quite short, which may not reflect the long-term impacts of RMT on athletic performance and changes in lung function. Furthermore, the participants comprised a varied population of basketball, rugby, and racing athletes, which may yield varying results depending on sports-specific demands.
Although all participants had sustained injuries below T1 level, they were not sorted by level of SCI. This would be a valuable consideration in future studies to give a more accurate insight into how training relates to breathing difficulties.
RECOMMENDATIONS
Future research needs to adopt performance-specific metrics (such as game-related sprint measurements and endurance analysis) in performance assessment. It is recommended to include assessments of heart rate variability, lactate threshold, or VO₂ max, as these can provide deeper insights into how heart rate–based recovery methods influence physical performance. The future studies will include comparisons with established RMT devices to contextualize the efficacy of this novel device against gold-standard interventions.
CONCLUSIONS
Respiratory muscle training enhances vital lung functions (FVC, FEV₁) together with respiratory muscle strength (MIP, MEP) while increasing endurance and propulsion effectiveness in wheelchair athletes. Training increased MIP and MEP, which indicated improvements in respiratory muscle strength. The observed benefits of RMT directly impact wheelchair athletes who need to optimize speed and stamina for enhanced recovery. Our findings indicate that regular application of RMT with regular training regimes can improve functional abilities and athletic outcomes in this group.
It is important to note that this trial is a modest one, and any results should be viewed as preliminary and intended to generate further research. While the findings are encouraging, they need to be reviewed in larger studies before they can be applied to other wheelchair athletes.