INTRODUCTION
Women with disabilities face multiple difficulties in accessing and participating in sports, including societal stereotypes, limited access to adequate facilities, and insufficient support for inclusive programs1. Misconceptions about their physical capabilities, and the male-dominated culture of sports, often discourage their involvement2. In addition, female Paralympic athletes experience minimal media representation and a shortage of adequately-trained coaches, further limiting their visibility, access to role models, and opportunities for equitable participation and recognition3-4.
The menstrual cycle was also long considered a barrier to female participation in sports. Historically, women were often discouraged from engaging in physical activities during menstruation due to concerns about their health and performance5. Currently, the menstrual cycle is not considered a limiting factor for sports participation, but the hormonal fluctuations throughout the cycle can impact athletic performance6. During the follicular phase, when estrogen levels are higher, women may experience increased strength and flexibility, as well as improved aerobic performance7. In contrast, during the luteal phase, elevated progesterone levels can contribute to a decrease in strength and may also influence body composition8. The increased progesterone levels may increase water retention, leading to temporary weight gain. Additionally, increased appetite during this phase, often accompanied by cravings for high-calorie foods, may theoretically lead to increased body fat9.
Female athletes with disabilities are more prone to gaining body fat compared to their non-disabled counterparts due to several factors. Reduced physical activity, resulting from physical limitations, leads to lower calorie expenditure, increasing the likelihood of fat accumulation. Additionally, many athletes with disabilities have reduced muscle mass, which lowers their metabolic rate and makes them more susceptible to fat gain10. Certain disabilities, like spinal cord injuries or neurological conditions, can disrupt weight regulation and metabolism, while some medications used for managing these conditions can also contribute to weight gain11.
For athletes engaged in high-level competition, effective menstrual management is a priority, particularly when it comes to mitigating symptoms such as dysmenorrhea and heavy menstrual bleeding, without compromising body composition12. The ideal contraceptive should preserve or enhance athletic performance by avoiding increases in fat mass or losses in lean mass. Research indicates that low-androgenic monophasic combined oral contraceptives (COCs) tend to influence body composition and may even support muscle maintenance13. Progestin-only methods, such as the hormonal intrauterine device (IUD), are also favoured by some athletes due to its localized effects and reduced systemic hormonal exposure. These methods offer effective symptom control with fewer metabolic side effects14.
While several studies have investigated the effects of hormonal contraceptives on athletes without disabilities, data on elite athletes, particularly those with disabilities, remain scarce13. Moreover, no previous study has specifically examined the impact of the levonorgestrel-releasing intrauterine device (LNG-IUD) on body composition in female paralympic athletes14. This represents a significant gap in the literature, particularly considering the increasing number of athletes opting for long-acting reversible contraception in preparation for major competitions. This study presents the first evaluation of the effects of the LNG-IUD on body composition in female paralympic athletes. Its aim is to better understand the implications of this contraceptive method in a high-performance population with unique physiological and training profiles, particularly in the context of preparation for the Paris 2024 Paralympic Games.
MATERIALS AND METHODS
Study design and participants
This prospective cohort study included 10 female athletes from the Brazilian Paralympic team, selected through convenience sampling. All participants trained at the national training center and were invited to participate via email, phone calls, and group discussions during team sessions.
The inclusion criteria were nulliparous athletes aged 19-27 years, actively competing in paralympic sports, and choosing the LNG-IUD for contraception. The exclusion criteria were abnormal uterine bleeding and spinal cord injuries above T6. Athletes with spinal cord injuries above the T6 level were not included in the study, as IUD insertion must be performed in a hospital setting due to the risk of autonomic dysreflexia during the procedure.
Procedures
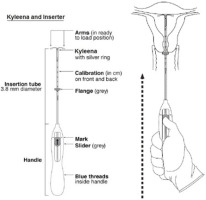
The LNG-IUD (Kyleena®, 19.5 mg levonorgestrel) was inserted following manufacturer’s guidelines. The athletes provided written informed consent to take part, and the study received ethics approval (IRB No: 6.215.943).
Before insertion, the athletes were informed about the efficacy, risks and the procedure itself. The device was inserted on an outpatient basis, preferably within the first seven days of the menstrual cycle, or at any phase of the cycle, after confirming the absence of pregnancy (Figure 1).
Outcomes
Body composition was measured using Dual-Energy X-ray Absorptiometry (DXA Lunar Prodigy Advance (GE Medical Systems, Madison, WI, USA) at the Brazilian Paralympic Training Center15. The body composition assessment was performed in the morning, prior to training sessions, after a four-hour fasting period. The participants were instructed to wear loose fitting clothes without any metal. Following this, the participants were positioned on the DXA-bed in a supine position with Velcro bands used to help keep the legs still during measurement. The total body scan was used to determine the following outcome measures: body mass, fat mass, body fat percentage, lean tissue mass and lean tissue percentage. Bone mineral density (BMD) of the spine and femur were determined after the body composition assessment and expressed in g/cm².
Menstrual cycle phases were systematically monitored in all athletes prior to the insertion of the LNG-IUD. While it was not always possible to perform all DXA assessments exclusively during the early follicular phase, efforts were made to schedule most of the tests within this phase to minimize hormonal variability. The phase of the menstrual cycle at the time of each examination was recorded and considered a potential source of variation in body composition measurements. After one year of LNG-IUD use, most athletes presented with either minimal or absent menstrual bleeding, which is consistent with the expected effect of the contraceptive; as such, continued cycle phase monitoring was unnecessary for follow-up assessments.
Statistical Analysis
Data were analyzed via the Statistical Package for Social Sciences (SPSS) (version 25, IBM, Chicago, Illinois, USA). A descriptive analysis was performed, including minimum and maximum values, percentiles, medians, means, and standard deviations. Comparisons between baseline and 12-month follow-up were performed using the Wilcoxon signed-rank test. To complement the p-values, the effect size was calculated using the rank-biserial correlation coefficient, providing a measure of the magnitude of differences observed. Statistical significance was set at p = 0.05.
RESULTS
The age of the athletes ranged from 19 to 27 years, with a mean age of 23. All the athletes were track and field competitors with at least five years of experience.
Table 1 presents descriptive data regarding the type of disability, age and body composition of each participant. Three athletes had intellectual disabilities, three visual disabilities and four physical disabilities. Among the athletes with physical disabilities, two presented with spastic cerebral palsy, while two exhibited upper limb hemiplegia secondary to obstetric brachial plexus injury. All athletes had body mass index (BMI) values within the adequate range according to current World Health Organization (WHO) guidelines, which define a normal BMI as between 18.5 and 24.9 kg/m² for the general adult population.
Table 1
Distribution of paralympic athletes by disabilities and body composition parameters
Figure 2 shows the individual changes in fat mass and lean mass of each participant before and after one year of hormonal IUD use.
Figure 2
Individual changes in fat mass and lean mass (kg) of each participant over the one-year period of hormonal IUD use
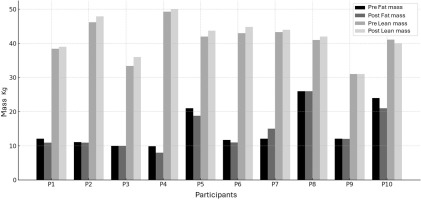
Table 2 compares body composition and bone mineral density values between baseline, i.e. before the insertion of the Kyleena IUD, and after one year of use. A statistically significant increase in lean mass was observed (p = 0.04), but no significant reduction in fat mass (p = 0.14). Although bone mineral density also increased after one year of hormonal IUD use, this change was not statistically significant (p = 0.46).
Table 2
Body composition values (total mass, fat mass, lean mass) and BMD, before and after one year of Kyleena IUD use in the 10 Paralympic athletes
| Variable | Before IUD | After IUD | p value |
|---|---|---|---|
| Total Mass (kg) | 58.3 ± 8.7 | 58.7 ± 7.8 | 0.53 |
| Fat Mass (kg) | 15.0 ± 6.2 | 14.4 ± 5.8 | 0.14 |
| Lean Mass (kg) | 40.9 ± 5.5 | 41.8 ± 6.6 | 0.04* |
| BMD (g/cm²) | 1.25 ± 0.1 | 1.26 ± 0.2 | 0.46 |
DISCUSSION
The use of the 19.5 mg LNG-IUD (Kyleena®) appears to be associated with favorable changes in body composition among female Paralympic athletes, particularly with regard to an increase in lean tissue mass. Such an increase in lean mass is notable for these athletes, as muscle mass is a key determinant of strength, endurance, and mobility16.
The increase in lean mass observed in this study is especially beneficial for individuals with cerebral palsy. DXA assessments show that these athletes generally have a lower amount of lean mass compared to athletes with other disabilities, and lower levels of total body fat. However, a higher proportion of visceral fat was observed, a factor that may increase the risk of developing cardiometabolic diseases17.
The decrease in fat mass and slight increase in BMD suggest that the LNG-IUD may support the optimization of body composition without the adverse effects associated with another hormonal contraceptives18,19. This is an important consideration for athletes, who often face unique challenges related to body composition, including a higher propensity for fat mass accumulation due to reduced physical activity levels in some disability groups20,21.
The increase in bone mass observed after one year of use of the Kyleena IUD, although not statistically significant, is also a relevant clinical finding for athletes, who often have a higher risk of osteopenia and osteoporosis. Early intervention is essential to preserve bone health and promote athletic longevity22. In individuals with hemiplegia secondary to obstetric paralysis, studies show that the affected limb has significantly reduced bone mineral density compared to the contralateral limb¹. In this context, contraceptives that do not negatively impact BMD are preferable to methods with deleterious effects, such as depot medroxyprogesterone acetate; fortunately, the hormonal IUD has minimal effects, even in disused limbs23.
Our research focused on track and field Paralympic athletes with physical disabilities, specifically those with spastic cerebral palsy and upper limb hemiplegia. The relationship between body composition and performance in this population is multifactorial, being influenced by the type of disability, event specialization, and training adaptations. Morphological characteristics such as BMI, fat mass, body fat percentage, and lean mass are significantly associated with physical and physiological performance. A study conducted with 66 male Paralympic track and field athletes with different disabilities (cerebral palsy, amputation, short stature and intellectual disability) showed that morphological characteristics, such as arm span and body fat index, influence motor performance. The article highlights that amputees and short stature athletes performed better in jumps and sprints24. Although our study evaluated only women and did not include any short stature athletes, our findings nevertheless provide further knowledge about body composition in Paralympic track and field athletes.
A strength of our study was the use of DXA, considered the gold standard for assessing body composition. DXA provides accurate measurements of lean mass, fat mass, and bone mineral density, making it particularly valuable for research in athletic populations15. DXA is also important for screening bone health risks in female paralympic athletes with low energy availability, which can lead to REDs syndrome25. Moreover, in athletes with hemiplegic cerebral palsy, a preserved BMD in the affected limbs, indicating that high-performance training can mitigate the negative impacts of the disability on bone mass26. These data reinforce that DXA should be considered a standard tool for monitoring health and performance in athletes with disabilities, with specific adaptations according to the type of disability and sport modality.
Continuous monitoring of body composition is essential for identifying nutritional imbalances, injury risks, and overall health trends. Strength-based sports benefit from increased muscle mass, while endurance sports require a more balanced body composition. These factors highlight the importance of body composition assessment in optimizing training and nutritional strategies for athletes 22.
Hormonal contraceptives can influence body composition, with effects varying depending on the formulation, dosage, and individual response27. Combined oral contraceptives have been associated with increased fat mass and fluid retention, which may negatively affect athletic performance28. Similarly, depot medroxyprogesterone acetate, a progestin-only injectable contraceptive, has been associated with weight gain and reduced bone mineral density, making it a less favorable option for athletes14. The LNG-IUD, with its lower systemic effects compared to oral pills or injections, helps preserve ovarian cycle integrity and supply metabolic benefits, such as maintaining bone mass. While some users report weight gain and fat redistribution, these changes are primarily attributed to fluid retention, a common effect of progestins29.
After one year of using the Kyleena IUD, the study observed an increase in lean mass, a reduction in fat mass, and improved bone density. These results differ from those using the Mirena IUD, which delivers a higher dose of levonorgestrel and resulted in an increase in fat mass and a decrease in lean mass. Besides the hormone dose, the difference may be explained by the fact that our study involved trained paralympic athletes, whose intense routines likely protect body composition; this highlights that both the hormone amount in the IUD and the user profile influence effects on lean and fat mass.
This study is the first such investigation of the use of the LNG-IUD specifically in Paralympic athletes. These athletes face unique challenges, including the need to optimize body composition for performance while managing the physical and hormonal demands of disabilities. The LNG-IUD, with its androgenic properties and minimal systemic effects, may offer a unique advantage for this population by supporting lean mass preservation and overall body composition.
While our study provides valuable insights into the effects of the LNG-IUD on body composition in Paralympic athletes, it has several limitations. The small sample size (n = 10) limits the generalizability of the findings, and the lack of performance data prevents us from drawing conclusions about the impact of these body composition changes on athletic performance. Future studies should include larger, more diverse samples of Paralympic athletes and incorporate performance metrics to better understand the relationship between body composition and athletic outcomes. Additionally, long-term follow-up studies are needed to assess the sustained effects of LNG-IUD use on body composition and overall health in this population.
In conclusion, these preliminary findings suggest that the levonorgestrel-releasing intrauterine device (LNG-IUD) may contribute to the preservation of lean body mass in female Paralympic athletes. However, given the exploratory nature of these results, larger and controlled studies with performance-related outcomes are necessary to confirm its potential benefits.