INTRODUCTION
Hypertension (HTN) is a medical condition characterized by a persistent rise in blood pressure (BP) within the blood vessels, It is a common cause of death and disability globally1 and often known as the silent killer. According to the World Health Organization (WHO), HTN is responsible for about half of the mortality attributable to heart disease and stroke, which affects one in three adults globally. By 2025, it is predicted that 1.56 billion people will have HTN.
Hypertension exists in both primary and secondary forms. Ninety-five percent of persons with high blood pressure have primary, or essential, hypertension, a condition for which there is no identified cause2. In Egypt, hypertension is a serious health problem that affects 26.5% of the population, or about 15 million individuals3. Essential hypertension is often accompanied by other cardiovascular hazards, including aging, diabetes, obesity, insulin resistance, and hyperlipidemia. Hypertension also increases the risk of dementia, chronic renal disease, aneurysms, heart failure, and stroke or heart attack: this elevated risk has been attributed to the arteries thickening and hardening as a result of high blood pressure, or other circumstances that typically occur only after long periods of uncontrolled hypertension4.
The cardiovascular system is controlled by vascular endothelial cells which produce several powerful local vasoactive substances, such as the vasoconstrictor peptide endothelin and the vasodilator molecule nitric oxide. Indeed, endothelial dysfunction has been linked to essential hypertension in humans, and endothelial function modification is a promising treatment strategy for reducing some of the major consequences of hypertension. It seems that reduced nitric oxide generation can be restored with clinically effective antihypertensive medication5.
Uncontrolled hypertension has been associated with poor sleep quality and circadian rhythm. Hypertensive patients have reported to demonstrate 70% poorer sleep quality, while blood pressure control positively impacted sleep quality. Sleep quality affects various physiological events that influence blood pressure such as autonomic nervous system function6, 7.
Older patients with HTN demonstrate poorer quality of life (QoL) than healthy individuals, which has been attributed to the symptoms of HTN8. Both mental and physical well-being contribute to overall health-related quality of life (HRQoL), and are significantly impacted by chronic disorders such as HTN9. Low control rates may be linked to complicated HTN symptoms and declining QoL10.
It is advised that hypertension should be effectively managed to reduce the risk of stroke and heart attack. Unfortunately, long-term use of anti-hypertensive medication lowers QoL. nevertheless, hypertension patients can control blood pressure (BP) by combining non-pharmacological treatment with antihypertensive medications11.
Transcutaneous electrical acupoint stimulation (TEAS) is a non-intrusive substitute for manual and electroacupuncture therapy, with the acupoints being induced by transcutaneous electrical nerve stimulation (TENS) rather than needles. It has the advantage of being incredibly simple to learn and unlike traditional acupuncture, it does not have any unfavorable side effects, such as infection or punctures of internal organs12. Previous studies have found TENS to decrease systolic blood pressure (SBP) and increase NO concentrations to high levels at acupoints13. Nitric oxide (NO) is known to be a significent modulator of local vascular tone and blood flow. Furthermore, by stimulating the vagus nerve, TENS can quickly lower high BP, and low-frequency TENS stimulation causes the release of endogenous opioids by the autonomic nervous system14.
Research indicates that TEAS is a non-invasive, low-cost, high-quality, and easy-to-use modality in managing patients with HTN. TEAS may impact the BP by protecting cardiac tissues and by controlling autonomic nervous system activity and lowering sympathetic activity15.
Modern acupuncture is based on traditional Chinese medicine (TCM), which posits that an imbalance in a person’s qi or energy can cause illness; acupoint stimulation can therefore regulate physiological reactions by sending signals to the brain and associated organs via nerves and Qi channels. Nevertheless, acupuncture has been shown to affect autonomic nervous system function, reduce BP, and enhance sleep quality in hypertension. Certain psychological characteristics, like anxiety and depressive symptoms, have often been linked to QoL; studies have examined this topics in hypertensive patients16.
Low-frequency TENS has been found to activate the opioid mechanism, which raises beta-endorphin and met-encephalin levels. The procedure has been found to alleviate pain; this has been attributed to it causing the midbrain to release an endogenous opiate (encephalin) and encouraging relaxation that enhances sleep quality17.
The aim of the study was to determine the impact of electroacupuncture on blood pressure, sleep quality, and QoL in patients with primary hypertension. The treatment may represent an alternative therapeutic modality to antihypertensive medications, which have complications and adversely affect sleep and quality of life with long-term use. Transcutaneous electrical nerve stimulationis a simple inexpensive approach that appears to have no obvious adverse effects14.
MATERIALS AND METHODS
Study design and participants
This single-blinded randomized controlled trial included 40 patients of both sexes with primary hypertension. They were selected from the Internal Medicine clinics at Menouf General Hospital, Menofia governorate, Egypt, from May 2024 to August 2024. The research was presented to the Research Ethics Committee of Physical Therapy, Cairo University in May 2024 (Approval code No.: P.T.REC/012/005510). Informed consent was gained from all participants before commencing the study, Clinical trials.gov identifier: NCT06401278.
The inclusion criteria comprised patients with primary hypertension, aged between 50 to 60 years old and BMI from 24.9 to 34.9 kg/m². All had been diagnosed by a specialist physician with primary hypertension at least six months previously, with systolic blood pressure (SBP) of 140–159 mmHg and/or diastolic blood pressure (DBP) of 90–99 mmHg. All were medically stable and under the control of prescribed antihypertensive medications.
The exclusion criteria comprised patients with secondary HTN, cardiac disorders (e.g., heart failure, recent myocardial infarction, atrial fibrillation, coronary artery disease, and left bundle-branch block), previous CABG surgery, implantable cardiac pacemaker, uncontrolled hypertension, any metal implants at the site of the application of TENS, dermatological disorders at the site of the application of TENS, diabetes mellitus, and current smokers.
Randomization
The participants were randomly distributed into two equal groups (n = 20). The study group (A) received transcutaneous electrical acupoint stimulation (TEAS) plus routine medical therapy, whereas the control group (B) underwent routine medical therapy only. The TEAS program was applied for 40 minutes per treatment session, three times weekly for six consecutive weeks.
Intervention
Transcutaneous electrical acupoint stimulation
The study group (A) received the TENS mode applied at specific acupuncture points using an electroacupoint stimulation device (EV-906 TENS/EMS, SN 21366136, NEW TAIPEI CITY TAIWAN)18. TEAS is a modern technique that integrates the effect of acupuncture point stimulation and TENS12.
Procedure
Each patient was instructed to assume a relaxed, comfortable, supine lying position. The procedures of the TEAS technique were explained clearly to the patient. The TENS adhesive electrodes1 were applied bilaterally to the following specific acupoints: Sanyinjiao (SP6), which is located at 3 cun (width of four fingers, not counting the thumb just over the tip of the medial malleolus on the posterior tibial margin; the cun is a relative unit of measurement used in traditional Chinese medicine to locate acupuncture points on the body. The other electrodes were applied to Taichong (LR3), which is located 2 cun (width of the middle three fingers) above the space between the first and second metatarsal bones on the dorsal aspect of the foot, and Nei-Guan (PC6), which located 2 cun above the mid-wrist creases between the tendons of the flexor carpi radialis and palmaris longus muscles19. The intensity was set to the highest acceptable level that did not result in pain or discomfort, and the TENS parameters were adjusted to have a frequency of 4 Hz and a pulse width of 200 μs20. The TEAS program was applied for 40 minutes per treatment session, three times weekly for six consecutive weeks.
Routine medical treatment
All study participants received the prescribed antihypertensive medication (Captopril-25 mg) administered twice daily. The patients were advised to eat a diet rich in fiber and potassium and low in salt, limiting their sodium intake to a maximum of 2,300 mg daily, and reducing sugar and fat. Other lifestyle modifications included avoiding using any products that contain nicotine or tobacco, such as cigarettes and chewing tobacco, identifying the sources of stress and finding ways to manage it through deep breathing or making time for fun activities, and avoiding alcohol consumption or smoking21. Usual sleep care was recommended, including setting a regular time to go to bed and wake up each day, and turning off electronic devices at least 30 minutes before bedtime22. This routine program was prescribed with follow-up for all patients who participated in the study.
Outcome measures
Blood pressure
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured for all patients at the start of the study and after six weeks of the intervention, using a digital sphygmomanometer (OMRON HEALTHCARE CO, Ltd. KYOTO.617-0002 JAPAN). Briefly, the patient sat on a chair with a back support for five minutes. Following this, the sphygmomanometer cuff was placed almost an inch above the antecubital fossa on the patient’s right upper arm. Blood pressure was then measured three times and the mean value was recorded to ensure reliability23.
Heart rate (HR)
Heart rate was measured using a pulse oximeter (20537 Hamburg, Germany), an electronic device that clips onto a patient’s finger24.
Nitric oxide (NO)
Three milliliters of venous blood were drawn from the antecubital vein of each patient. An SN 801754821 spectrophotometer (BioSystems S.A.Costa Brava, 30080030 Barcelona, SPAIN) was used to estimate blood NO content after separation of serum by centrifuge25.
Pittsburgh Sleep Quality Index (PSQI)
All patients were tested using the Pittsburgh Sleep Quality Index (PSQI). This is a valid and trustworthy self-assessment tool that provides information on daytime dysfunction, sleep latency, duration, typical sleep efficiency, sleep trouble, usage of sleep pills, and sleep quality over one month. The answers are scored on a scale of 0 to 3. The total score for all seven sections creates a single global score. A total score of five or more denotes a “poor” sleeper26.
SF-12 health status questionnaire
The quality of life physical component score (PCS) and mental component score (MCS) were evaluated using the short-form SF-36 tool. This includes eight scales and 12 items: perceived mental health, role limitations because of emotional problems (RE), role limitations because of physical problems (RP), physical functioning (PF), vitality (VT), bodily pain (BP), general health (GH), and social functioning (SF). Better health is indicated by higher ratings on the SF-36 and SF-12 scales, which range between 0 and 10027.
Sample size calculation
The necessary sample size was calculated via the G* Power software (version 3.1.9.4), and relied on the mean lowering of SBPobserved in prior studies28, 29. The mean SBP in the TEAS group was 112.94 ± 13.52 mm Hg and was decreased by approximately 9% (an absolute change of 10.26 mm Hg) compared to the control group (123.2 ± 6.4 mm Hg). The total determined sample size for the present study was 36 with a 0.97 effect size, 80% power, and α level of 0.05 at the two-tailed level (t-tests: Means: Difference among two independent means—two groups). Therefore, the total required sample size was 40 (20 per group), accounting for a potential 10% drop-out.
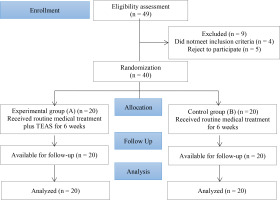
Assessment of eligibility: A total of 49 patients were initially contacted. Of these patients, five declined to take part in the trial, and four did not meet the inclusion criteria. The final 40 patients were distributed into two equal groups (20 patients each). All assigned patients underwent follow-up and statistical analysis.
Statistical analysis
Data were analyzed via the Statistical Package for Social Sciences (SPSS) (version 25, IBM, Chicago, Illinois, USA). Categorical variables were displayed as frequencies and percentages (N) and analyzed using the chi-square (χ2) test or Fisher’s exact test. For continuous variables, the Shapiro–Wilk test was initially performed to evaluate the normality of their distribution. The data were found to be normally distributed and hence were displayed as means and standard deviations (SD). An independent t-test was employed to compare the two groups’ variables, including SBP, DBP, HR, NO, PSQI, the SF12 physical component score (SF12 PCS), and the SF12 mental component score (SF12 MCS). Also, a paired t-test was used to evaluate the change from pre-intervention to post-intervention. Effect sizes were quantified using reported partial eta squared values (ηp2) (< 0.01 = small, 0.06 = moderate, and 0.14 = large). With a comparable 5% error margin, the confidence interval was 95%. Statistical significance was set at p < 0.05, highly significant at p < 0.001, and insignificant at p > 0.05.
RESULTS
The study included a sample of 40 patients with primary hypertension. The participants’ demographic characteristics are displayed in Table 1. No statistically significant differences were noted between groups with regard to age, sex, weight, height or BMI (p > 0.05).
Table 1
Demographic characteristics of patients of the two groups
Both the TEAS and control groups demonstrated statistically significant reductions in mean SBP, DBP, HR, and PSQI score from before to after six weeks of intervention. Before the intervention, no statistically significant differences were noted between groups; however, after treatment, the TEAS group exhibited significantly lower SBP, DBP, HR, and PSQI scores compared to the control group (p < 0.001) (Table 2).
Table 2
Within and between-group statistical analysis of SBP, DBP, HR, and PSQI before and after intervention
The TEAS group exhibited a significant increase in NO, SF12 PCS, and SF12 MCS from baseline to six weeks after intervention (p < 0.001); however, no such changes were noted in the control group (p = 0.162, 0.297, and 0.495, respectively). Before treatment, no significant changes were observed between groups; however, after treatment, the TEAS group demonstrated significantly higher NO, SF12 PCS, and SF12 MCS compared to the control group (p < 0.001) (Table 3).
Table 3
Within and between-group statistical analysis of NO, SF12 PCS, and SF12 MCS before and after intervention
DISCUSSION
The aim of this study was to determine the impact of electroacupuncture on BP, sleep quality, and quality of life in patients with primary HTN. The results indicate significant intragroup differences, i.e. between pre- and post-intervention, for all measured variables in the TEAS group, but only for SBP, DBP, HR, and PSQI score the control group. At the post-intervention point, all evaluated variables were found to be significantly more favorable for the TEAS group, which had lower (SBP, DBP, HR, PSQI) and higher (NO, SF12 PCS, SF12 MCS) than the control group.
Several alternatives exist to traditional needle acupuncture, including magnetic acupressure, auricular therapy, electroacupuncture (EA), laser acupuncture, acupressure, and transcutaneous electrical acupoint stimulation (TEAS)29. TEAS is a method that integrates the impact of acupuncture with transcutaneous electrical nerve stimulation (TENS) by stimulating acupoints with electrode pads30. Similarly to our current findings, Tu et al.31 found home-based TEAS to elicit a greater reduction in SBP (mean, −8.53 mm Hg) than in a control group (−1.70 mm Hg); the authors conclude that adding home-based TEAS to standard hypertension patient care was safe, acceptable, and a potential therapeutic option.
TENS may potentially offer further benefits for lowering BP in hypertensive individuals who do not respond well to medication: one study found treatment to reduce BP for one week following the intervention32.
Moreover, Kamali et al.33 found TEAS to significantly lower systolic and diastolic BP, i.e. SBP and DBP, in hypertensive patient when applied at specific acupuncture points, namely PC5, PC6, LI4, and LI10. It is believed that BP is elevated in hypertensive patients due to autonomic nervous system dysfunction, which is marked by hyper sympathetic nervous system activation34. As such, promoting the parasympathetic nervous system, inhibiting the sympathetic nervous system, and enhancing the proper function of the autonomic nervous system may lower blood pressure by causing the heart to contract less and the systemic blood vessels to dilate; it has been suggested that this may be achieved by the use of TENS at acupuncture locations35.
Zhang et al.36 reported thatfor both normal patients and those with increased BP, electrical stimulation of acupoints decreased SBP, but not DBP. In addition, stimulating point PC6 for 30 minutes decreased systolic blood pressure in hypertensive patients by 11%35. Studies also indicate that Acu-TENS may have a vagal inhibitory influence on HR following exercise training.
The present findings were also consistent with a previous study comparing the impact of acupuncture on BP and HR in cases with essential HTN and normotensive individuals; the study investigated the impact of acupuncture on vagal nerve activity and cardiac sympathetic nerve activity (CSNA) based on heart rate variability (HRV). The findings suggest that acupuncture may lower the BP and HR by increasing vagal nerve activity in cases with mild to moderate HTN. When the patient has a baseline sympathetic tone that is greater than usual, the efficacy of acupuncture appears to be more noticeable37.
Our present findings are in line with those with Tsuchiya et al.38 who report that stimulation of Li4, P6, P8, L6, and H5 acupoints by acupuncture needles enhances local circulation by elevating nitric oxide (NO) levels in the treated areas. No is an important modulator of local vascular tone and blood flow.
Other findings indicate that TENS-induced acupoint stimulation promotes NO production. Improved NO activates guanylyl cyclase to generate cGMP (cyclic guanosine monophosphate), and cGMP provides smooth muscle relaxation and vasodilatation, which improves local microcirculation13. TENS, acupuncture, and acupuncture-like TENS modify blood nitric oxide levels, arterial blood pressure, and localized cutaneous blood flow39.
Our results are in accordance with Bang et al.40 who investigated the efficacy of low-frequency electrical stimulation on persistent insomnia. A combination of subjective evaluations and electroencephalogram (EEG) measures found electrical stimulation to improve sleep quality: sleep latency decreased, total sleep duration increased, and the severity of the insomnia also fell. This data suggests that low-frequency TENS a safe and successful therapy option for chronic insomnia. Indeed, acupuncture and Acu TENS have been found to influence both the sympathetic and parasympathetic nervous systems, which may induce sleep. Moreover, acupuncture may enhance levels of the inhibitory neurotransmitter, gamma-aminobutyric acid (GABA), thus improving sleep41.
Patients with hypertension who experienced sleep disturbances also reported markedly reduced QOL, especially in the physical domain, indicating that improving sleep quality positively affects blood pressure control and enhances quality of life6.
It has been proposed that as the TEAS may have an analgesic effect by activating endogenous pathways. Electrical stimulation can can initiate endogenous opioid release in the brain and spinal cord via the nervous system; these substances include endorphins, enkephalins, and dynorphins, and directly inhibit opioid-sensitive spinal cord interneurons42. Additionally, it has been shown that applying TENS on muscles raises skin temperatures and blood flow, which encourages relaxation and improves QoL and sleep43.
Hypertension significantly impacts both the mental and physical aspects of QoL, and this effect can be exacerbated by the presence of complications44. Indeed, Lazuardi et al.45 report that patients with essential HTN who received press needle therapy to stimulate acupoints in addition to antihypertensive medications had lower blood pressure and better QoL scores than those who only received antihypertensive medications. Furthermore, acupuncture is widely used to treat psychological aspects, including anxiety and depression, and improve quality of life46.
Conversely, a study of the impact of TENS on PC5 and PC6 acupoints in healthy subjects; found HR, SBP, and DBP to increase during the session but fell soon after. The findings also indicate an intra-session increase in sympathetic tonus, and a decrease in parasympathetic autonomic tonus, indicating that TENS application has an influence on HR and BP in healthy individuals34. Also, Lazaro et al.47 report that using low-frequency stimulation TENS had no considerable impact on BP in healthy humans, regardless of its intensity.
Strengths and limitations
This study has a number of advantages. It was performed as a randomized controlled trial to examine the effects of electroacupuncture on blood pressure, sleep quality, and quality of life (QoL) in patients with essential hypertension. Additionally, the inclusion of a control group allows the precise effect of the interventions to be determined in contrast to standard medical care. The findings indicate that TEAS is a non-invasive method that can help regulate blood pressure, improve quality of life, and reduce insomnia in primary hypertension patients.
The study also has some limitations. Firstly, the sample was rather small, and is restricted to a particular age range and physical condition; as such, it may not accurately reflect the general population with HTN. Furthermore, the brief follow-up period might not adequately reflect the long-term impact of therapy. Therefore, we recommend carrying out additional research with larger sample sizes and a wider range of age groups. These studies should also compare the effects of TEAS with those of other modalities in future research.
CONCLUSIONS
In individuals with primary hypertension, transcutaneous electrical acupoint stimulation (TEAS) appears to lower blood pressure and enhance sleep and quality of life; it hence appears to be a novel, simple, and inexpensive adjuvant to standard medical treatment with no obvious adverse effects. It may improve physical functioning, raise psychological well-being, and lower the morbidity rate of hypertension. Hence, it is recommended as a conservative strategy for inclusion in treatment programs aimed at patients with primary hypertension.