INTRODUCTION
One of the most prevalent problems associated with the musculoskeletal of the upper body is forward head posture (FHP). In FHP, the head is displaced anteriorly to the vertical axis, thus moving the centre of gravity forward and raising the stress on the posterior neck. This posture alters force couplings and scapular movements, resulting in tissue overuse, damage, and pain, and impacting scapular mechanics and muscle activation surrounding the shoulder complex1.
Studies based on craniovertebral angle measurement suggest that FHP affects approximately 62.1% of university students, which has been attributed to their prolonged use of computers and smartphones, and poor posture2. This configuration shifts the wight forward on the cervical spine, altering the mechanical stress on the spine and exacerbating several neck-related musculoskeletal problems3. As a result, the occipital muscles shorten and the cervical lordosis increases. It also results in inappropriate and continuous activation of the occipital, cervical, and shoulder muscles, as well as a relative compensatory action; this weakens the deep cervical flexor muscles (DCF) which decreases neck stabilization and induces neck pain (NP)4.
Forward head posture is also frequently associated with uncontrolled movement (UCM) patterns; these represent a contributing factor to NP symptoms, which impair neck functions and compress the joint on one side while producing tensile strain on the other. Failure to address UCM may result in a variety of symptoms, including movement control dysfunction, and ultimately various tissue pathologies due to the associated tissue tension and stress5.
Kinetic control (KC) is term used to describe movement executed with the best possible balance between physiological stressors and neuromuscular control. It requires the action to be performed with the correct timing and amplitude, and with the appropriate intensity. Together with determining the location and direction of the UCM, KC is a crucial component in treating symptomatic FHP is retraining based on direction-movement control (DMC)5.
Common treatments for symptomatic FHP are cervical and thoracic spine mobilization, soft tissue mobilization and massage, cervical and scapular stabilization exercises, and postural education6. However, little data currently exists on the results of including cervical and shoulder kinetic control training for participants with symptomatic FHP.
This aim of the study was to determine the impact of supplementary cervical and shoulder KC training on deep cervical flexor endurance (DCFE) (motor control), craniovertebral angle (CVA), NP, and neck disability index (NDI) in people with symptomatic FHP.
MATERIALS AND METHODS
Design
The study was performed as a single-blinded randomized controlled trial with two arms in parallel. The researcher performed the measurement, gave instructions to participants, and conducted the intervention. The research conformed to the Declaration of Helsinki guidelines for human subjects. It was authorized and approved by the research ethics committee (ID number P.T.REC/012/005328) at the Faculty of Physical Therapy, Cairo University, as well as the clinical trial registry databases (ID number NCT06586463). The study was conducted between September 2024 and January 2025.
Participants
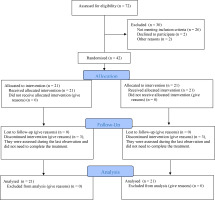
The study included 42 participants, aged between 18 and 40, of both sexes, with symptomatic FHP < 50°7 (Figure 1). All were recruited through word-of-mouth, i.e. oral requests to participate from the colleges and staff of the Faculty of Physical Therapy, Cairo University. Participants were not involved if they had previous neck injuries, neck and shoulder surgery, shoulder trauma, tendinitis, or thoracic surgery7. All participants provided their informed consent before taking part.
Randomization
The participants were randomized into either Group A (control group) or Group B (experimental group) with a 1:1 allocation ratio. The allocation used computer-generated blocks (blocks of four) to minimize bias and variability between the two groups. The participants were assigned sequential numbers to ensure hidden allocation, with randomization codes being kept confidential in transparent, sealed envelopes.
Outcome Measures
Craniovertebral angle (CVA)
The CVA was measured using Kinovea software; this has been found to be a valid and reliable tool with good intra-rater reliability and high ICC values (≥0.80), with a confidence Interval (CI) of 95%8. A 64-megapixel camera (Samsung A52)9 was situated on an adjustable tripod 80 cm from the participant (Figure 2), with the base set at shoulder height. The participants were requested to stand in their typical upright posture with their hands relaxed at their sides and to flex and extend their necks to relax, gaze forward, and maintain stability. Two adhesive labels were put on the tragus of the ear and the C7 spinous process (Figure 3). From the dominant side, three lateral view photos were captured. The CVA was calculated based on the line from C7 to the ear tragus and the horizontal line from C7, with the mean of the three angles provided. A normal CVA is considered to be greater than 50°10.
NP intensity measurement using the numerical pain rating scale (NPRS)
The NPRS is a valid and reliable scale for evaluating pain severity with ICC = 0.76 (95% CI: 0.51–0.87). The participants indicate their pain severity along a horizontal line marked from 0 to 10: 0 (no pain) and 10 (the worst pain)11.
NF measurement using the Arabic neck disability index (NDI)
NF was evaluated using the NDI, a valid and reliable tool with an excellent ICC at 0.96 (95% CI: 0.93–0.97). NDI scores range from 0 to 50, where 50 represents complete disability and 0 represents no activity limitation. The respondent indicates their responses to statements on a six-point scale ranging from 0 (no disability) to 5 (complete disability). The index is calculated as a percentage by summing the scores, dividing the total by the maximum possible score, and multiplying the result by 10012.
Deep cervical flexor endurance (DCFE), i.e. the primary outcome, was assessed by the Cranio-cervical flexion test (CCFT) with a pressure bio feedback unit (PBU)
DCFE was evaluated using the CCFT test, a valid13 and reliable method with perfect intra-rater reliability (ICC values between 0.71 and 0.96) and moderate to nearly perfect inter-rater reliability (ICC values between 0.54 and 1.0)14. The test evaluates the capacity to initiate and maintain isolated cranial and cervical flexion while in a supine position (Figure 3). The measurements were taken using a Stabilizer pressure biofeedback unit (PBU) (Chattanooga, USA). Briefly, an inflated PBU (20 mmHg) was positioned beneath the neck. The participants then initiated and maintained isolated cervical and cranial flexion (CCF) for 10 seconds at increasing pressure values (22, 24, 26, 28, and 30 mmHg) while performing the CCF test. The maximum pressure that could be maintained with proper form was recorded. The performance index was then calculated by multiplying this maximum pressure value (i.e. activation score) by the number of correct 10-second holds that the participants could complete at that pressure (activation score × number of successful repetitions); for example, if a participant could achieve the second level of the test (24 mmHg) and perform 6 10-s holds with the correct CCF action, then the performance index was 4 × 6 = 24. The performance index ranged from 0 to 100. A normal response is for the participant to sustain the position for 10 seconds at 26-30mmHg without using the superficial cervical muscles15. During the exercise, the therapist palpated the neck to identify undesired stimulation of the superficial cervical muscles.
treatment Procedures
The intervention was carried out by the corresponding author. This researcher has years of experience and holds a certificate in kinetic control.
Group A (control group) received conventional therapy comprising cervical stabilization exercises16 and scapular stabilization exercises17 for four weeks; briefly, each exercise was held for 10 seconds with 10 seconds rest, with 10 repetitions per set based on participant tolerance. The exercise was performed for 30 minutes a day, three times a week18. A hot pack was applied for 10 minutes a day as part of the home program, and the participants followed the provided posture correction instructions 19. Participants also practiced stretching exercises that targeted the sternocleidomastoid, scalene, and pectoralis minor muscles; each stretch was held for 30 s, followed by a 30 s rest period. Three repetitions were performed for each muscle on each side20.
Group B (experimental group) underwent the same treatment as the control group, plus lower cervical (LC) and shoulder KC. The LC UCM correction was based on a structured upper cervical flexion (nodding) exercise program. The exercise program started with the LC spine positioned neutrally, with the occiput and the scapulae supported by a small folded towel to put it in a neutral position. As control improved, the exercises progressed to positions with reduced support, such as standing5.
For shoulder UCM correction, the participant stood with the scapula supported against a wall, and was instructed to raise their shoulders upward, backward and then slightly downward, and maintain this position while raising their arms as much as possible. the exercise was performed while the participant stood with the scapula supported against a wall and The elbow was kept flexed to shorten the arm lever length and lessen the load. As control improved, arm flexion was executed unsupported through the partial range that could be well controlled. The exercise was eventually progressed to the full benchmark range, 90°, with the elbow straight. Visual, auditory, and kinesthetic cues were provided to help participants become familiar with the task without scapular movement or glenohumeral translation. The exercise began with a single limb and then progressed to both limbs5.
The KC protocol was performed three times weekly for four weeks. Each set comprised ten repetitions, each held for ten seconds. Initially, the exercise was performed for at least two to three minutes about two sets per day, then progressed according to tolerance5.
sample size estimation
Sample size was estimated using G*POWER software (version 3.1.9.4), the calculation used t-tests for Wilcoxon-Mann-Whitney test (two groups) was applied, with α = 0.05, Power = 0.95, Allocation ratio = 1, and effect size d = 1.79. The results indicated a minimum sample size of 20; therefore, assuming a dropout rate of 20%, 24 participants should be recruited. This effect size was calculated from a pilot study on 20 participants (10 in each group), with DCFE as the primary outcome. However, the actual sample size used was 42, consisting of 21 participants in Group A and 21 participants in Group B.
statistical analysis
Quantitative variables were examined for normality using the Shapiro-Wilk test. As the data were not normally distributed, non-parametric testing was used for the analysis. Values were displayed as median, minimum, and maximum for quantitative variables, or as numbers and proportions for qualitative variables. The chi-square test or Fisher’s exact test was used to compare qualitative characteristics (sex) among treatment groups. Between-group comparisons were performed using the Mann-Whitney test, and within-group comparisons using the Wilcoxon signed-rank test. Statistical significance was assumed for p<0.05, and all tests were bilateral. The analysis was performed using IBM-SPSS software version 27.
RESULTS
The participant characteristics for all groups are given in Table 1. No significant changes were detected between the two groups regarding median age, weight, height, or sex distribution (p > 0.05). However, BMI differed significantly between groups (p < 0.05) pre-intervention.
Table 1
Participants’ characteristics (both groups)
| Measured variable | Group A Median (IQR) | Group B Median (IQR) | Mann-Whitney U Median (IQR) | P-value |
|---|---|---|---|---|
| Age (years) | 20 (4) | 19 (3) | 178 | 0.277 |
| Weight (kg) | 63 (9) | 68 (20) | 271.5 | 0.199 |
| Height (cm2) | 168 (18) | 167 (14) | 224.5 | 0.920 |
| BMI (kg/m2) | 22 (4) | 24 (18) | 304 | 0.035* |
| Sex distribution | N (%) | N (%) | ||
| Women | 13 (38.1%) | 12 (57.1%) | 0.753 | |
| Men | 8 (61.9%) | 9 (42.9%) | ||
Both groups demonstrated significant within-group changes in median CCFT, NDI, CVA and NPRS over the course of the programme (p < 0.001; Wilcoxon signed-rank test). (Table 2; Mann-Whitney U-Test), although Group B demonstrated superior outcomes in CCFT and NDI. No significant differences in median CVA or NPRS were found between the groups post-intervention.
Table 2
Within and between-group variable differences
| Measured variable | Group A pre Median(IQR) | Group A post Median(IQR) | Group B pre Median(IQR) | Group B post Median(IQR) | Between-group difference in improvement (P-value) | Within-group difference (P-value) |
|---|---|---|---|---|---|---|
| CVA in degrees | 45.5 (5.5) | 50.5 (8.2) | 46.2 (7.6) | 51.9 (4.2) | 0.204 | <0.001* |
| NPRS | 7 (2) | 4 (2) | 7 (3) | 3 (2) | 0.990 | <0.001* |
| NDI (%) | 22 (15) | 12 (10) | 26.6 (16) | 10 (9) | 0.010* | <0.001* |
| CCFT in mmHg | 6 (8) | 24 (24) | 8 (8) | 50 (48) | 0.012* | <0.001* |
DISCUSSION
Our findings indicate significant improvements in DCFE and NDI during the intervention, with more favourable results observed for the kinetic group than the control group. However, no significant difference in CVA or NP was observed between groups post-intervention, as they demonstrated equal effectiveness.
These findings also demonstrate that adding LC and shoulder kinetic control exercises led to significant improvements in DCFE and NDI. These enhancements improved neuromuscular control and reduced maladaptive movement patterns. The intervention targeted movement directions that individuals struggle to control, promoted correct motor control, reduced strain on cervical structures, and restored proper muscle activation and coordination. This justification is corroborated by a study of the long-term impacts of DMC training on chronic nonspecific neck pain (NP) by Khosrokiani et al.21, who note significant improvements in NP, NDI, functional endurance and DCFE in the DMC group compared to the control group; however, no significant improvement in NP was noted in the present study.
Our DCFE and NDI findings agree with those of a study of students with chronic NP with improper posture by Lee et al.22, who examined the effect of deep flexor strengthening exercises. The findings reveal significant improvements in posture and CCF compared to the control group, who took part in basic stretching. Improving neck and shoulder posture necessitates the strengthening of DCF muscles, which play an important role in adjusting neck posture and ensuring neck stability.
The current DCFE results are also in line with those of Jull et al.23, who found that specific low-load CCF exercises improved DCF muscle activation and coordination in people with chronic NP. The low-load program targets motor control by training coordination between neck flexor muscle layers and improving CCF movement quality.
In contrast, our findings regarding DCFE and NDI are in disagreement with Falla et al.24, who examined whether neck flexor strengthening exercises and low load CCF affected DCF activation. The study indicated no significant change between groups regarding the change in relative latency of DCF activation during the intervention. This implies that a shift in muscle activation might not always result from enhanced muscular function attained with various training methods, such as functional postures and tasks.
Our findings on CVA and NP are consistent with those of Sikka et al.25, who studied 30 individuals with both NP and FHP and who routinely used computers. Their data indicated no significant change in CVA or NP in the experimental group (receiving DCF training and postural education) compared to control group (receiving postural education only). Therefore, it does not appear that engaging a single muscle group in isolation can be advantageous, as this may result in a muscular imbalance surrounding the cervical spine. Addressing the muscle imbalance is important to allow optimal flexibility of the tight muscles.
Another study in forward head posture compared the effects of callisthenic exercises (CE) with motor control exercises (MCE), three times a week for four weeks. The study included thirty individuals aged 18 to 40. Statistically significant improvements in CVA within the two groups. Between-group comparisons indicated similar improvements in CVA and CCFE. Both CE and MCE were found to correct muscle imbalance, and to have a positive impacting CVA and postural stability in individuals with asymptomatic FHP. Their data agree with our present findings with regard to CVA, but not DCFE26.
Interestingly, a study by Suvarnnato et al.27 contradicts our present observations regarding CVA and NP, but confirm those regarding NDI. A total of 54 individuals were assigned to three groups at random: one group received deep cervical flexor (DCF) muscle training, another semispinalis cervicis training (SCT) training targeting the deep cervical extensor muscles, and the control group received standard therapy, which included general exercises and modalities. Both study groups showed significant improvements in CVA, an indicator of improved head posture, when compared to the control group. Certain deep cervical muscle activities may help reestablish sensorimotor control of the cervical spine and enhance neuromuscular function.
The inclusion of cervical and scapular stabilization exercises in the current study may explain the improvements in the control group. A systematic narrative review of 16 RCTs by Yang et al.6, found that postural correction exercises and manual therapy effectively reduced pain and disability in individuals with FHP. The authors recommend exercises targeting cervical and scapular stabilization to improve posture, decrease muscle strain and fatigue, and restore cervical spine stability, thereby reducing pain and disability.
When interpreting the results of our study, some limitations should be considered. The treating physiotherapist was not blinded to the group allocation, and the sample was small; in addition, no follow-up was performed to evaluate the long-term effects of treatment. Hence, there is a need for additional research with larger sample sizes.
CONCLUSIONS
It was found that supplementing standard physiotherapy treatment with cervical and shoulder KC in participants with symptomatic FHP improved the DCFE (motor control) and NF more effectively than standard treatment alone. While both groups experienced improvements in CVA and reductions in NP, indicating that each treatment approach was beneficial, the KC group demonstrated superior outcomes in motor control and NF, suggesting that incorporating KC into FHP management may offer additional therapeutic advantages.