INTRODUCTION
Pes planus, or flatfoot, has many symptoms and levels of deformity. It is caused by altered loading of the medial aspect of the feet and the plantar arches. In weight-bearing conditions, flatfoot manifest as a lowered medial longitudinal arch (MLA), a pronated subtalar joint, and a valgus alignment of the calcaneus1. One of the most prevalent varieties of flatfoot is flexible flatfoot, characterised by an arch in the open kinetic chain but not in the closed kinetic chain.Individuals with flexible flatfoot may exhibit postural problems, along with weakness and exhaustion in the foot and leg; this will result in diminished bodily effectiveness, early onset of fatigue, back discomfort, and subsequent deformities in an individual2.
Approximately 10% to 25% of the population has flatfoot to some extent3. Individuals with flatfoot exhibit more instability than those with normal arches during static standing, and those with flexible flatfoot have lower static and dynamic stability. However, despite the impact of flatfoot on body positioning, little research has been conducted on their impact on balance4.
Balance is the mechanism by which postural stability can be maintained. Static balance is operationally defined as the ability to keep a posture in various positions, such as standing or sitting, while dynamic balance is regarded as the ability to preserve postural control during movements, such as walking or reaching an object. Both static and dynamic balance are considered essential for motor abilities5.Having flatfoot can result in several issues, beginning with improper posture, which leads to the deterioration of muscles and joints, and ultimately to chronic discomfort in the feet, ankles, knees, hips, and back6.
Multiple studies examined the strategies intended to enhance balance in individuals with flatfoot, including short foot exercises (SFE)7, one-legged dynamic balance training8, and the use of kinesiotape to reinforce the medial longitudinal arch9. SFE is a widely employed technique for enhancing postural stability and reinforcing the plantar muscles. The short foot is a foot posture characterized by an elevated MLA, whose aim is to enhance the biomechanical placement of the foot7.Pilates training is a comprehensive body conditioning practice originally designed for alleviating low back pain and enhancing stability in the elderly10; it represents a physical training methodology that emphasizes posture, flexibility, segmental alignment, and core stability through specific postural and movement exercises11.
Although various balance-training procedures have been implemented to enhance postural stability, no studies have yet evaluated the potential of dynamic balance training in patients with flexible flatfoot using Pilates training; in addition, no data exists regarding the effect of Pilates training on improved quality of life improvement in flexible flatfoot. As such, the aim of the present study is to determine the effect of Pilates training on improving dynamic balance and quality of life in patients with flexible flatfoot.
MATERIALS AND METHODS
Design
A single-blind, pre-post randomized controlled study was performed in individuals with flexible flatfoot to evaluate the impact of Pilates on dynamic balance, including front average deviation, back average deviation, left average deviation, and right average deviation, as well as on quality of life.The study was approved by the Research Ethics Committee of the Faculty of Physical Therapy, Cairo University (reference number P.T.REC/012/005435), and adhered to the principles outlined in the Declaration of Helsinki on human research. The trial was recorded in the clinical trial registry (registration number: NCT06539533). The research was performed from October 2024 to December 2024.
Participants
A total of 44 university students (10 men and 34 women) were recruited from the Kafr Elsheikh University Faculty of Physical Therapy. All participants had a bilaterally pronated foot posture and were aged between 18 and 21 years12; body mass index (BMI) ranged from 18.5 to 2513. The following exclusion criteria were applied: recurrent lower extremity injuries, including fractures or deformities, or a history of surgical intervention in the lower extremities; any neurological deficit affecting balance; any medication that can affect balance; pregnant and breastfeeding women; and participants with unilateral flexible flatfoot14.
Randomization
Each participant was informed of the purpose, rationale, and benefits of the study, and were told that they can freely with draw from study at any time according to their will. All participants gave their consent to take part by signing a consent form, in accordance with the Helsinki protocol.
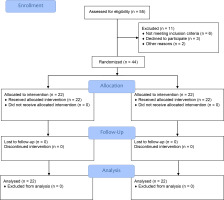
The participants were assigned into two groups using a random generator. The primary author oversaw the randomization process and did not participate in evaluation or treatment. The randomization codes were maintained in a sealed opaque envelope to maintain confidentiality. The final author evaluated the outcome measures while remaining blinded to the allocation and treatment procedures. Both groups took part in five-week programmes: Group A (22 individuals) performed Pilates training bi-weekly 10,15 combined with short foot exercises for three minutes daily11, while Group B (22 individuals) only engaged in short foot exercise for three minutes daily 16 (Figure 1).
All outcome measures were evaluated at baseline, i.e. before the intervention began, and immediately after the treatment ended.
The flatfoot was assessed using the navicular drop test (NDT) to identify alterations in the height of MLA. NDT is a valid and reliable test with intra-rater reliability with ICC > 0.88017,18. The participants were instructed to sit in a chair with the knee joint flexed at 90°, ensuring the second toe aligned with the knee to position the subtalar joint neutrally. The distance from the ground to the navicular tuberosity was measured and documented using a ruler under non-weight-bearing conditions. The distance from the ground to the navicular tuberosity was measured in a standing position, with the feet placed shoulder-width apart and weight distributed evenly on both feet. The disparity in the height of the navicular tuberosity between sitting position and standing position was assessed. If the discrepancy exceeded 10 mm, the person was classified as having flexible flatfoot19.
Dynamic balance was assessed for all participants using a Balance Check 636 stability tester (Dr. Wolff, Arnsberg, Germany), a validated device20,21 ; itsprotocolwasexplainedtoeach participantprior totheevaluation. The device consists of a multi-axial standing platform, i.e. a Sensbalance Mini board, which can be tilted up to nearly 360 degrees, connected to a computer which calculates front average deviation, back average deviation, right average deviation, and left average deviation, and presents the data in real time. Briefly, the participant stands for 30 seconds on both legs on the wobble board, with their feet about 15 cm apart, without shoes or socks on and with their eyes open. The participant then follows the on-screen instructions (Figure 2).
The participant was informed that an alarm would sound, and the platform would become unstable immediately afterwards; following this, they had to maintain a stable position for the whole duration of the test. The participants had to concentrate on the screen in front of them and try to keep the cursor (i.e. the centre of the platform) in the centre of the bullseyeon the screen while standing on the unstable platform20.
Quality of life was assessed using the Arabic version of the foot function index (FFI) questionnaire: the FFI is recognized as the most prevalent assessment instrument for foot-related complaints. This instrument is considered feasible, readily calculable, comprehensible to participants, and requires fewer than 10 minutes to complete22. The FFI consists of 23 items categorized into three subscales: pain (nine items), disability (nine items), and functional restriction (five items). The participants are directed to complete the questionnaire based on their experiences from the past week. The final score is obtained by summing all the scores and dividing the total by the maximum possible value; this value is then multiplied by 100 and rounded to an integerbetween 0 and 100. Higher scores imply poor foot health and quality23. The test-retest reliability of FFI-Arabic version was found to be good to excellent, with intraclass correlation coefficients ranging from 0.8 to 0.9322.
Treatment procedures
Pilates training
The Pilates protocol consisted of 30 minutes of exercises, comprising five minutes of warm-up, 20 minutes of Pilates exercises, 10 repetitions for each exercise with 10-20 seconds of rest between each exercise, and five minutes of cool-down. The warm-up and cool-down comprised brisk walking/jogging, breathing exercises, and stretches to facilitate recovery and reduce injuries and discomfort24. The exercises were performed twice a week for five consecutive weeks10. Pilates were performed under supervision with a proper breathing pattern. The Pilates exercises used in the study comprised the articulating bridge, hundreds, plank10, rolls up, one-leg stretch, and lift leg supine24.
1-Articulating bridge: The participants were instructed to lie supine with their feet flat on the floor (knees bent) and arms positioned beside their bodies. They were instructed to withdraw their stomachs and to start peeling the vertebrae off the floor sequentially, starting with the coccyx. The motion concluded once reaching the scapula; this position was maintained for three seconds. The participants thereafter returned to the initial position. Participants breathed in preparation for the maneuver and exhaled while elevating their body. Inhaled at the apex of the posture and expelled throughout the descent.
2-Hundreds: The participants were instructed to lie supine with their arms positioned alongside their bodies and their pelvis in a neutral alignment. They were directed to elevate their head and shoulders from the floor while flexing both hips and knees of the lower limbs at a 90-degree angle.They were then instructed to retract the abdomen while raising the arms and lowering them gradually, beginning the motion at the shoulder joint. The participants inhaled for a five count and exhaled for another five counts.
3-Plank: The participants assumed a plank position, with both forearms in contact with the ground, forming fists with their hands and maintaining 30 cm between their elbows.They sustained 90-degree angles at the ankles. They then engaged the abdomen utilizing the abdominal drawing-in movement, while keeping the shoulders and hips elevated 25 cm from the ground. The participants were instructed to breathe consistently while executing the plank, and to sustain it for fifteen seconds25.
4-One-Leg Stretch (Single-Leg Stretch): The participants were asked to place their head, scapulae, and one knee into their chest while lying supine in the chest lift position. Then, the participants were asked to extend the straight leg as high as possible while keeping the lower back in contact with the mat. The participants were instructed to breathe in, bending the extended leg and then extending the bent leg. The participants exhale as their leg fully straightens out and the hand transfers to the other knee.
5-Roll-Up: The participants were instructed to lie flat with their legs straight and together, their arms directly overhead, parallel to their shoulders, and their palms facing forward. They then inhaled, pulling the abdominal wall inward toward the spine. Following this, they elevated the head and scapulae from the mat, extended the arms toward the ceiling, and drew the chin toward the chest; this movement was accompanied by dorsiflexion of the ankle and foot. The participant exhaled, curling upward and transitioning from a seated position until the upper body is elevated above the legs, with fingers directed toward the toes. They then inhaled until the sacrum contacted the mat and began to roll back downward. Upon completing the rolling motion, they elevated their arms above their head and returned to the starting position.
6-Leg lift supine: The participants assumed a crooked lying position with their feet flat on the mat and hip-width apart. Their palms faced downward, and their arms resting alongside their bodies. They exhaled while elevating one leg until the thigh was perpendicular to the mat, keeping a 90-degree angle at the knee joint. They then inhaled, maintaining the 90-degree angle at the knee joint and lowering the leg until the toes contacted the mat.
Short foot exercise (SFE)
All participants were directed to attend a training session at the beginning of the exercise treatment, where they were instructed on the proper technique for executing the SFE by the researcher. Each participant was required to demonstrate the correct technique without compensatory extrinsic muscle involvement prior to concluding the training session.
All participants were directed to elevate the MLA of the feet by retracting the metatarsal heads towards the calcaneus without flexing the toes andmaintain an isometric contraction for five seconds during each repetition. Each participant executed the SFE for three minutes daily over a span of five weeks: each session consisted of three sets of 10 repetitions, with each repetition sustained for five seconds, totalling approximately 30 repetitions16; in addition, a 45-second rest period was added between sets26.
Every participant was directed to perform SFEs at home daily, for a duration of five weeks; making a total of 35 home workouts. Each week, the participants were required to document their home workouts on a diary sheet, while the second author conducted follow-up communications via phone messages to verify compliance with the program. After five weeks, 85.7% of patients in Group A and 88.6% in Group B had complied with home exercises.
Power analysis
The sample size was determined using balance, as outlined in Kim27, with 80% power at an α level of 0.05, including two measurements for two groups and an effect size of 0.47; the calculation used F-test MANOVA for repeated measures within and between interactions. It was found that the minimum necessary sample size was 38 participants, with an additional 6 (15%) people accounted for as potential dropouts, resulting in a total sample size of 44 participants, i.e. 22 in each group. The sample size was determined utilizing G*Power software (version 3.0.10).
Statistical analysis
The Shapiro-Wilk test was used to confirm the normality of the data and Levene’s test for homogeneity of variances and assess group homogeneity. The data had a normal distribution, and the variance was homogenous. The unpaired t-test was employed to compare groups based on all demographic data. The impact of treatment on front average deviation, back average deviation, right average deviation, left average deviation, and FFI were analysed using mixed MANOVA. Upon obtaining significant findings from the MANOVA, further univariate ANOVAs were performed. Posthoc testing employing the Bonferroni correction was conducted for multiple comparisons. The significance level for all statistical tests was set at p=0.05. All calculations were performed using SPSS version 23.
RESULTS
Demographic characteristics
The characteristics of groups A and B are given in Table 1. No statistically significant differences regarding were found between groups (p-value ≥ 0.05).
Table 1
General characteristics of patients (n = 44) *
The impact of treatment on the assessed variables was evaluated using a mixed-design multivariate analysis. A statistically significant difference was noted between groups for all studied parameters: Wilk’s A = 0.67, F (5, 38) = 3.69, p-value < 0.001, Partial Eta Squared (ƞ2) = 0.33. In addition, a statistically significant effect was also noted for all parameters regarding time (i.e. pre-post treatment): Wilk’s A = 0.03, F (5, 38) = 278.95, p-value < 0.001, ƞ2 = 0.97. A significant effect was also observed for the interaction between groups and time: Wilk’s A = 0.13, F (5, 38) = 49.37, p-value < 0.001, ƞ2 = 0.87.
Within-groups comparison
All outcome measures demonstrated significant changes when comparing pre- and post-intervention findings (p-value < 0.0001) in groups A and B, as illustrated in Table 2.
Table 2
Within and between group analysis for dynamic balance and FFI (n = 44) *
Between-groups comparison: Baseline and after five weeks of intervention
At baseline, no significant differences were found between groups for any measured variable (p-value ≥ 0.05; Table 2). However, after five weeks of intervention, significant intergroup differences were observed for all assessed variables, favouring Group A (p-value < 0.05; Table 2).
DISCUSSION
In flatfoot, the sustained pronation of the heel causes the talus bone to shift inward, lowering the medial longitudinal arch (MLA), and diminishing the capacity to distribute weight. Subtle biomechanical changes in the support surface may affect postural control strategies. As the arch begins to collapse, balance at the feet is compromised, which disrupts overall body balance27.
Our present study found that the combination of a 5-week Pilates training regimen, consisting of two sessions per week, with short foot exercises (SFE), produced statistically significant improvements in dynamic balance and quality of life compared to controls, who only performed SFE.Significance improvements in dynamic balance and quality of life were noted between the groups, with a greater improvement noted in the Pilates + SFE group. This may be because Pilates has been found to be more effective than static stretching for improving flexibility28.This significant finding implies that executing a Pilates training program can strengthen the regulation of trunk movement and improve the neuromuscular coordination of movements and lower limb strength; it can also improve the dimensions of pain, difficulty, and physical activity limitations10.
Our findings align with those of Jiang et al.29, who compared Pilates training (PT) to standard balance training (BT) in 51 collegiate football players with chronic ankle instability: 26 in the (PT) group and the remainder in the (BT) group. The groups engaged in training as designated three times weekly for a duration of six weeks. The authors conclude that Pilates-based core stability training is a more effective preliminary intervention for patients with acute ankle sprains who are unable to perform progressive ankle strengthening exercises due to pain and symptoms, compared to traditional balance training. The authors attribute this to the fact that Pilates is a sensory proprioceptive training that utilizes open and closed kinetic chains, and one that focuses on maintaining proper alignment throughout the entire movement. As a result, during the exercises, the continuous stimulation of the proprioception of the ankle and foot joints in the closed kinematic chain is emphasized, while improving the arch of the foot and correcting the malformation of the calcaneus-valgus in the flexible flatfoot. Proprioceptive exercises play an important role in developing positional reflective circuits, which are essential for creating proper confidence in foot placement during static and dynamic positions; in turn, this improves balance and functional mobility30.
Taner et al.31 assessed the impact of Pilates exercises on body structure and dynamic balance performance in inactive women. The study consisted of 16 volunteer participants aged 21 to 44. The women in the experimental group (n = 8) engaged in a 45-minute Pilates regimen three times weekly for a duration of eight weeks. The women in the control group (n = 8) maintained their everyday routines throughout the eight-week duration. The statistical analysis indicated that the eight-week Pilates exercise program enhanced body structure and dynamic balance in inactive women.
Also, Kim et al.32 report that the Pilates Hundred enhances core muscle activation, resulting in an effective exercise program for individuals seeking to improve core muscle volume, function, and rehabilitation. According to Preeti et al.10, dynamic balance requires stable posture to be maintained over the base of support, and it is an important fitness component to prevent lower limb injuries caused by poor balance; Pilates exercise training was found to be successful in improving spinal alignment and core muscle strength. The Pilates training was found to have a significant impact on quality of life; in addition to body-mind training, Pilates practice is believed to provide a pleasurable movement experience, which may add to its appeal to consumers seeking psychological well-being. According to studies, physical activity promotes health and can provide pleasant sensations of pleasure and satisfaction while also lowering anxiety and sadness33.
Hyun et al.34 investigated the effects of mat Pilates and balancing exercises performed on an unstable base of support on trunk stability and balance in older women. Forty participants aged 65 or older were evenly divided into a Pilates mat exercise (PME) group and an unstable support surface exercise (USSE) group. They engaged in exercise three times a week for a duration of 12 weeks, with each session lasting 40 minutes. Both PME and USSE produced notable enhancements in both static and dynamic balance capabilities among the participants.
Mohamed et al.35 did research to assess the effects of Pilates exercises on lower limb muscular strength and balance in patients with healed lower limb burns. Seventy-six patients of both sexes with thermal burn injuries were recruited. The participants were assigned to two groups, each consisting of 38 individuals: an experimental group participated in Pilates exercises alongside a conventional physiotherapy regimen, encompassing stretching, range of motion, and strengthening activities, while a control group participated solely in the conventional physiotherapy regimen. Both groups adhered to a treatment protocol consisting of 24 sessions over eight weeks, with three sessions each week. The researchers determined that Pilates exercises significantly improve lower limb muscular strength and balance in adult patients rehabilitating from second-degree thermal burns.
Our results indicate that while practising short foot exercises (SFE) alone was not as effective as the combination of short foot exercises with Pilates, the routine nevertheless significantly improved dynamic balance in individuals with flexible flatfoot. This may be attributed to SFE enhancing neuromuscular activity by stimulating the neurocircuitry in the sole, hence improving postural and core stability. Foot strength is thought to impact somatosensory regulation of standing posture and balance by influencing the muscle and tendinous receptors in the foot and ankle, particularly the plantar cutaneous receptors36. McKeon et al.37 established the ‘foot core system’, which connects intrinsic foot muscle (IFM) strength to core stability, proposing that an abdominal drawing-in movement can be paired with the SFE to improve total lower body stabilization.
Our results align with those of Moon et al.38 who investigated the immediate effects of SFE on the dynamic balance of individuals with (navicular drop of ≥10 mm). They found that SFE enhanced dynamic balance. SFE stimulates the proprioceptors in the feet, increasing friction between the plantar surface and the ground, which enhances afferent stimulation, thereby improving stability and voluntary muscle activities and stabilizing the MLA.Neuromuscular control of the intrinsic foot muscles is crucial for stabilizing the tarsal and metatarsal bones and regulating the rate of pronation. A study by Lynn et al.39 examined the effects of two types of IFM training (SFE and towel-curl exercise) on the height of the MLA and performance in static and dynamic balance tasks; of these, SFE demonstrated greater effectiveness in training the IFM.
In contrast, Rothermel et al.40 compared the efficacy of a traditional balance training program with a balance training program focusing on foot posture for improving postural control. They note that SFE may also be concentrated on maintaining foot posture during training and assessment, rather than just on balance, and that traditional balance training is more effective than balance training focused on foot positioning for enhancing postural control in healthy individuals. A comparison of the efficacy of jumping rope exercises and SFE on pain reduction and quality of life improvement in patients with flatfoot by Preeth et al.41 concluded that the combination of jumping rope exercise and ultrasound therapy produces better results in managing Pes Planus than SFE alone.The limited enhancement in dynamic balance observed in the SFE group may result from reduced sensory input due to the lack of perturbation while performing these exercises.