INTRODUCTION
Postural balance is described as the capability of the human body to maintain its equilibrium and to recover its balance as soon as the center of gravity shifts from the anterior of the second sacral vertebra1. Body position is maintained with respect to environmental surroundings and gravity by coordinating visual, vestibular, and somatosensory or proprioceptive sensory inputs2. Together, these inputs ensure optimal postural control, which plays a key role in avoiding fall-related traumas by maintaining the center of gravity.
Pregnancy is a natural phenomenon that encompasses a variety of biomechanical, physiological, body composition, anatomical and psychological changes in the mother. These changes, however, can impair balance and increase the risk of injury and falls3. This can also have implications for the pregnancy, as pregnant women hospitalized after a fall are more at risk of preterm labour than those who have not4.
During pregnancy, sleep disturbances increase from first to third trimester, and research has found poor sleep quality to impair postural balance during menopause5. Physical inactivity has also been recognized as an independent risk factor for pregnancy-related complications. The American College of Obstetricians and Gynecologists (ACOG) guidelines for physical activity during pregnancy indicate that pregnant women should perform at least 150 minutes of moderate-intensity aerobic physical activity per week, such as brisk walking, during and after their pregnancy: for example, 30 minutes a day, five days a week6. However, fear of falling can compel a pregnant woman to limit physical activity to avoid hazardous consequences, and most pregnant women fail to achieve the recommended routine physical activity levels7. These factors should not be overlooked while assessing postural balance among pregnant women.
Balance instability can be evaluated in a number of ways. For example, the functional capacity of the sum of multiple systems that enable postural stability can be determined using clinical measurement tools. Simple balance tests include the functional reach test, modified clinical test of sensory interaction on balance, timed up and go test, Romberg test and four-stage balance test; detailed balance tests such as the Berg balance test, Tinetti balance assessment tools and balance evaluation system can also be used.
While a number of methods are available for traditional balance training, these programs are not always successful in engaging participants over time8. Innovative balance training regimens can also be used therapeutically and have various visual feedback systems for more educational and research purposes; these include virtual reality, force platform and Biodex balance systems, among others9. These technologies have been shown to increase adherence to training protocols, and to stimulate cognitive abilities10, and can provide instructions and offer feedback on progression. One such device is the Biodex Balance System, which can objectively assess and improve balance while focusing on proprioception, somatosensory and neuromuscular control11.
Although falls are not uncommon during pregnancy, their incidence remains overlooked as literature regards maternal accidents as a direct cause of still birth; falls are also being increasingly recognised as a health concern12. As such, little is known of the combined effects of PA and sleep quality on postural balance in pregnant women. Therefore, the aim of the present study is to determine the relationship of postural balance with physical activity and sleep quality, and to identify the factors associated with postural instability in pregnant women.
MATERIAL AND METHODS
Ethical approval
Ethical approval was obtained from the Riphah Ethical Committee (Riphah/RCRS/REC/00833) of Riphah International University, Pakistan and the Ethical Review Committee of Foundation University Islamabad, Pakistan (FF/FUMC/215-65/Phy/20). The study was performed according to the ethical rules declared by Helsinki and World Health Organization. Ethical, cultural, and moral values were considered during the data collection procedure and written consent was obtained from all participants.
study design
This is a cross-sectional analytical study conducted on a sample of 138 pregnant women aged between 16 to 35 years over a period of seven months, from January to July 2021. A non-probability convenient sampling technique was used for the study. The sample size was calculated using G- Power software 3.1 for multiple linear regression, with 10 predictors, an effect size of 0.15 (medium effect), α= 0.05, and power (1-β) = 0.80. The minimum required sample was 118. Our final sample was chosen to ensure sufficient power to detect meaningful relationships in the regression model.
selection criteria
The study included women with normal pregnancy of any trimester. The following were regarded as criteria for exclusion: complicated pregnancy, use of medication affecting balance, a diagnosis of musculoskeletal impairment of the lower limbs, any diagnosed cardiovascular and neurological deficit.
Outcome tools
All the standard operating procedures and precautionary measures were taken into account during balance assessment. A brief obstetric history was taken prior to the balance and fall risk assessment. The primary outcome of study was postural balance, and the secondary outcomes comprised sleep quality and physical activity levels.
Postural balance
Postural balance and fall risk were objectively assessed using the Biodex Balance System; postural balance was assessed using postural stability and m-CTSIB, whereas fall risk assessment was assessed using the fall-risk test13.
For postural stability, the test protocol was set as 20 seconds for test duration, stability was set at level 8 with two leg stance. The result was calculated on three scores, viz. overall stability index (OAPSI), which calculated deviations in all directions, anterior/ posterior stability index (APSI), which showed deviations in sagittal plane, and medial/ lateral stability index (MLSI), which reported deviation in the frontal plane14.
The modified-clinical test of sensory interaction and balance (m-CTSIB) provides an objective assessment of the interaction between various sensory conditions while maintaining balance. Higher scores indicate poor balance. The m-CTSIB was divided into four conditions. Condition 1 was characterized by standing on a firm surface with both eyes open, with all visual, somatosensory and vestibular inputs remaining intact. Condition 2 was characterized by standing on a firm surface with both eyes closed, where balance is dependent upon somatosensory input. In Condition 3, the participant stands on a foam surface with the eyes open, where balance is dependent upon visual input. Finally, in Condition 4, the participant stands on a foam surface with both eyes closed, where balance is dependent upon vestibular input only15.
Fall risk was assessed using the Fall Risk Test (FRT). Performance was evaluated based on the final score, termed the stability index, with a higher score being suggestive of a greater risk of falling. The following protocol was used: test duration 20 seconds, Biodex Balance system stability level 12, for most static surfaces, or 8, for dynamic stability with a bilateral stance16.
Physical activity levels
Physical activity was estimated using the pregnancy physical activity questionnaire (PPAQ). The PPAQ included several questions, and the amount of time spent in 31 activities was recorded. The activities were divided into several categories depending upon intensity and type. Physical activity was divided into sedentary, light, moderate and vigorous intensity, and into household or caregiving, occupational and sports or exercise during the current trimester. Higher scores indicated better PA. The duration of time spent in each activity was multiplied by its intensity in METs to get the mean weekly energy expenditure (MET-h·week-1) specific to each activity; the total metabolic equivalent of the task per week was calculated by adding all the individual responses in the questionnaire17.
sleep quality
Sleep quality was estimated using the Pittsburgh sleep quality index questionnaire (PSQI). The PSQI consisted of nine questions that were scored to give seven component scores, viz. subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleep medication and daytime sleep dysfunction. All the components were summed to get a global score for sleep quality ranging from 0 to 21. Higher scores were indicative of poor sleep quality, with a cut-off value of five points18.
statistical analysis
Data analysis was performed using SPSS 21. Normality was tested using the Kolmogorov Simonov test: the data for maternal BMI, overall postural stability index (OAPSI), fall risk test (FRT), light intensity PA, occupation and PA levels were found to be normally distributed. Parametric tests were applied for normally distributed data, and non-parametric tests for data without a normal distribution. Overall postural balance and fall risk was reported using means and graphically through box plots. The differences in postural balance and fall risk scores between trimesters were assessed using one-way ANOVA and Tukey’s post hoc test. A p-value <0.05 was considered significant. Pearson’s correlation test was used to evaluate the relationship between parametric variables, and Spearman’s rank-order correlation for non-parametric variables.
To determine the predictors of postural balance, multiple linear regression was applied. The dependent variables included postural stability index, fall risk test score and m-CTSIB score were used as, measured on a continuous scale. The following independent variables were included: pre-natal physical activity, sleep quality and important demographic variables about clinical information of participants. The analysis also assumed an absence of outliers, a linear relationship between dependent and independent variables and an absence of multi-collinearity between independent variables. The models were adjusted for potential confounders, including maternal age and trimester, to control for their effects on postural balance. A p-value <0.05 was considered statistically significant.
RESULTS
The mean age of the participants was 27.20 ± 5.3 years with a range of 19-35. The mean body mass index was 26.25 ± 3.9 with a range of 18 to 34. Detailed demographics are given in Table 1.
Table 1
Demographics of the study group
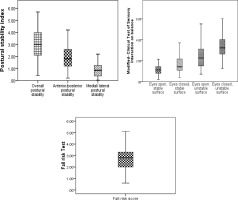
Mean overall postural stability index was 3.04 ± 1.24, and mean fall risk test 2.74 ± 1.02. The median m-CTSIB test value was 2.10 (IQR 1.28) (Figure 1).
A trimester-wise comparison of postural stability and fall risk (Table 2) indicated significantly higher scores in the third trimester compared to the second and first trimesters (p-value <0.05). However, the change in m-CTSIB scores between groups was insignificant (composite score p-value 0.07).
Table 2
Descriptive statistics (mean ± SD) for postural balance scores among groups
Median reported total physical activity was 151.53 (110.7) with a minimum of 6.65 and a maximum of 419.53 (Table 3). Of all 138 participants, 135 (97.8%) were classed as having sedentary PA, with a median score of 54.6 (61.8).
Table 3
Descriptive statistics for physical activity levels
Mean sleep quality, assessed using the Pittsburgh sleep quality index, was 9.14 ± 9.0 (Table 4). Overall, 108 (78.3%) participants reported poor sleep quality. The descriptive statistics of the seven components of PSQI are shown in Table 4.
Table 4
Descriptive statistics for Pittsburgh sleep quality index (PSQI)
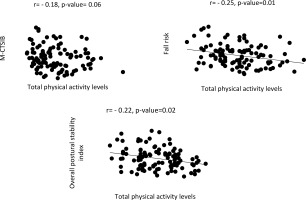
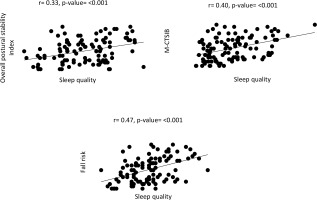
Correlational analysis was used to identify any significant relationship between postural balance, sleep quality, and physical activity (Figure 2 and 3).
The multiple linear regression analysis of the predictors of postural balance is presented in Table 5. Overall postural stability, fall risk and m-CTSIB were used as dependent variables, and trimester, occupation, gestational BMI, parity, mode of previous deliveries, past medical/obstetric history, history of previous falls, sleep quality and physical activity as independent variables. Occupation was categorized as (1) Working (formally employed or self-employed), (2) Student (enrolled in academic programs), and (3) Not working (homemakers or unemployed). Not working was used as the reference category.
Table 5
Predictors of postural balance
The full model summary indicates a good level of prediction, based on the R value; the adjusted R-square value indicates the percentage of the variability explained by the independent variables with regard to the overall postural balance scores. The regression model was found to be a good fit for the data, as shown in the ANOVA table. The variation of the dependent variable against a particular independent variable, assuming that all other independent variables remain constant, is given by the unstandardized coefficients in the coefficient table (β = 3.28 p < 0.001).
DISCUSSION
This analytical cross-sectional study examined postural balance, physical activity and sleep quality, and the relationships between them, in a group of 138 pregnant women. The findings indicate higher overall postural balance and fall risk scores among pregnant women; furthermore, this risk was greater during the third trimester than the second and first trimesters. The influence of sensory interaction on balance worsened by the third trimester but the difference was not statistically significant. In addition, most of the women reported poor sleep quality, and most were living a sedentary lifestyle. Postural stability was found to be significantly correlated with total PA, particularly sedentary, light intensity, household chores and occupational PA levels; significant correlations were also observed with overall sleep quality, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and use of sleep medication. Furthemore, PA level, occupation, fall history and habitual sleep efficiency were strong predictors of postural balance.
Similarly to our present findings, Inanir et al.14 also report postural balance to worsen by the third trimester. However, surprisingly, Inanir et al. also report poorer postural instability (0.78 ± 0.50) than the present study (3.04 ± 1.24), as well as a lower fall risk: 1.90 ± 1.10 compared to 2.74 ± 1.02 herein. The relatively poor postural stability noted in the present study could be attributed to greater anterior/ posterior and medial/lateral instability.
In contrast, another study found dynamic postural stability to be better in the third trimester than the second trimester Although the authors do not offer a potential reason for this difference, they suggest that factors other than perturbation and reaction time may be responsible; nevertheless, they report that few perturbations were administered to challenge the balance of the participants19.
Dunning et al.20 report a 26.8% fall rate among pregnant women. This is similar to the rate identified in the present study, where 29 (21%) of the participants reported having a fall history. However, while the previous study was conducted over email and telephone, the present study collected data in person.
Our findings indicate a significant relationship between physical activity and fall risk, where increased physical activity is associated with a decreased risk of falling. This stands in contrast with Klenk et al.21, who report no association between physical activity and fall risk. This variation could be attributed to the differences in the approaches taken to assess physical activity and fall risk. For example, unlike the present study, the previous study could not objectively measure fall risk.
Sousa et al. report that physical activity does not correlate with postural balance assessed by m-CTSIB22. A possible reason for this might be inadequate physical activity levels; indeed, our present participants were categorised as sedentary physical activity (PA). The American College of Obstetrics and Gynecologists recommend participating in moderate intensity PA for 30 minutes a week. This may suggest that the m-CTSIB is less sensitive to variations in physical activity levels, particularly among participants with predominantly sedentary behaviours. Future studies may consider using more dynamic sensory tests, or experimenting with dose-response effects of PA on sensory balance outcomes.
Our present findings also indicate a moderate positive correlation between sleep duration and postural balance. This is in line with Noh et al.23, who report that sleep, particularly sleep duration, is associated with an increased risk of falling.
Our data also indicate that occupation, prior falls and sleep efficiency are stronger predictors of postural instability than psychological elements. Similarly, a 2024 study by Shaikh et al.24 found that higher PA levels were not associated with reduced pain or better psychosocial outcomes in this population, and that other non-psychological factors may be more influential.
According to our present data, daytime sleep dysfunction appears to be an independent predictor of postural balance. This is confirmed by a previous study conducted on postmenopausal women5; however, unlike our present study, the previous study also found that postural balance may be affected by sleep duration and subjective sleep quality. The basis of these differences may lie in the physiological and hormonal changes particular to pregnancy.
The present study has some limitations. Firstly, as it excluded women with complicated pregnancies, the results cannot be generalized to all pregnant women. In addition, although the study includes several potentially confounding variables, namely gestational age, BMI, sleep quality and physical activity, some others were not addressed directly; these include footwear habits (use of supportive or non-supportive shoes), weight gain progression and environmental factors (flooring surface, home layout, lighting) throughout pregnancy. These variables should be considered in future research to improve applicability to real-life settings.
Nevertheless, the study highlights certain factors, viz. physical activity level, sleep efficiency, occupation status and previous fall history, that are potentially modifiable with appropriate therapeutic strategies, and can be used to highlight women at higher fall risk. Routine balance assessments can help integrate targeted interventions performed as part of antenatal programs during midwifery visits, physiotherapy referrals including structured PA guidance aligned with ACOG recommendations, and sleep hygiene education and support, with workplace and home safety advice for women with prior fall history or occupational demands. Even so, to properly formulate recommendations aimed at improving postural balance and reducing fall risk during pregnancy by focusing on pregnancy-specific lifestyle modifications, further research based around interventional studies is clearly needed.
CONCLUSIONS
Pregnant women are at a higher risk of falls due to increased postural instability, which is exacerbated by low PA levels and poor sleep quality. This poor postural stability, and hence elevated fall risk, is most prominent during the third trimester. Balance is significantly influenced by physical activity, occupation, fall history and sleep efficiency. It is recommended that postural balance should be evaluated during antenatal visits to avoid falls and fall-related traumas.