Introduction
Atopic dermatitis (AD) is a cutaneous, inflammatory, chronic, and relapsed disease, characterized by pruritus and eczematous lesions. Clinical manifestations range from mild and localized forms to severe and disseminated ones [1]. The prevalence of AD has steadily increased, affecting 7.9% of children between 6 and 7 years old and 7.3% of adolescents between 13 and 14 years old around the world [2].
The pathophysiology of AD includes the interaction of genetic, environmental and immunological factors, and in more than 50% of the cases, it is associated with other chronic diseases, such as asthma and allergic rhinitis [3]. Among the factors that trigger AD exacerbations, emotional stress is highlighted [4].
The symptoms of AD affect the quality of life (QoL) of patients and their families, mainly due to intense pruritus, unaesthetic appearance of lesions, sleep disturbances, and treatment expenses. Mental health of children and adolescents with AD has been studied in several countries, and it has already been observed that dermatosis contributes to the development of mental disorders (MD) [1, 5, 6]. In Spain, a total of 80 children with AD were evaluated using the instrument “Early Childhood Inventory-4” (ECI-4), and 69% of them were identified with some MD [6]. In the US, data obtained from telephone interviews on the health of 92,642 children with and without the AD diagnosis showed that children with AD have a higher prevalence of depressive disorder, anxiety disorder, behavioural disorder, autistic spectrum disorder and attention deficit/hyperactivity disorder (ADHD) when compared to their peers who were not affected by the disease [5]. In Brazil, the evaluation of 26 children with AD showed a risk of MD of 78% [7].
Studies indicate that siblings of children and adolescents with chronic diseases have an impairment in their mental health. The risk for them is up to three times greater than for the general population regarding behavioural and psychological problems [8, 9]. However, no publications on the evaluation of mental health of healthy siblings of children and adolescents with AD have been found so far.
The high risk of MD in the paediatric age group demands health professionals to use techniques to identify the need for evaluation and treatment of mental health. One alternative for the professionals to improve their skills in identification and, consequently, to enable the early referral of children and/or adolescents with indications of MD is the use of validated scales. The Child Behaviour Checklist (CBCL) is an example of these scales [10]. It is a large questionnaire considered to be the gold standard. It is supposed to be answered by parents and/or guardians, based on routine activities and family and social relationships, in order to provide an analysis of the emotional, social and behavioural profile of the child and/or adolescent.
Aim
The current study aimed to determine the risk of MD in children and adolescents with AD and to compare it with the risk of MD in their respective healthy siblings.
Material and methods
This study was cross-sectional research aimed to evaluate the risk of MD in children and adolescents with AD and their respective healthy siblings through prospective data collection. A non-probabilistic, convenience and systematic sample was used to select the participants.
Participants and measures
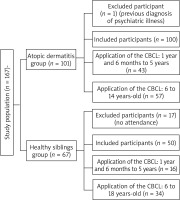
All children and adolescents who fulfilled the clinical criteria for AD (atopic dermatitis group – ADG) according to the classification of Hanifin and Rajka [11] were selected. They were seen on two afternoons per week in a tertiary-level hospital. To evaluate the other group (healthy siblings group – HSG), healthy siblings with no clinical diagnosis of AD and other serious chronic diseases were included. Children and adolescents with a previous diagnosis of MD and in follow-up for psychiatric illness were excluded (Figure 1).
The risk of MD was determined using the instrument CBCL (validated for the Portuguese language) [10]. The CBCL in two versions (pre-school – between 18 months to 5 years/school – between 6 years and 18 years) is indicated to evaluate children and adolescents. It is answered by parents and/or guardians. The version used to evaluate children between the age of 18 months and 5 years contains specific themes for the pre-school age group, being composed of 100 questions that evaluate the following syndromes: “Emotional Reactivity”, “Anxiety/Depression”, “Isolation” and “Somatic Complaints”, which constitute internalizing problems when grouped together. “Attention Problems” and “Aggressive Behaviour” are grouped as externalizing problems. The syndrome “Sleep Problems” is evaluated separately. The version used to evaluate students between the age of 6 years to 18 years is composed of 113 questions classified in eight syndromes: “Anxiety/Depression”, “Isolation” and “Somatic Complaints”, grouped as internalizing problems; “Rule-Breaking Behaviour” and “Aggressive Behaviour”, grouped as externalizing problems. The syndromes “Social Problems”, “Thought Problems” and “Attention Problems” are evaluated separately.
The CBCL consists of questions that should be answered as “absent/not true” (score = 0), “sometimes/slightly true” (score = 1) or “often true” (score = 2). At the end, it contains open-ended questions for parents. The sum of scores is converted into T-scores according to analyses that are appropriate for each sex and age. T-score below 64 is Normal; between 65 and 69, Borderline; and equal to or above 70, Clinical.
Results
A total of 150 children and adolescents – 100 with a clinical diagnosis of AD (ADG) and 50 healthy siblings (HSG) – participated in the study. The sample of parents and/or guardians who answered the evaluation instruments was composed of 83 (83.0%) mothers, 9 (9.0%) fathers and 8 (8.0%) grandparents.
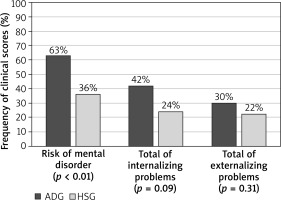
The ADG was composed of 45 (45.0%) male and 55 (55.0%) female participants, with median age of 6 years and 6 months (ranging from 1 year and 6 months to 14 years). The presence of risk of at least one MD classified by the CBCL was observed in 63.0% of this group. Internalizing problems were observed in 42.0% of the cases, and externalizing problems, in 30.0%.
The HSG was composed of 30 (60.0%) male and 20 (40.0%) female participants, with median age of 8 years and 5 months (ranging from 1 year and 7 months to 17 years-old and 5 months). The presence of risk of at least one MD classified by the CBCL was observed in 36.0% of this group. Internalizing problems occurred in 24.0% of the cases and externalizing problems, in 22.0% (Figure 2).
Figure 2
Risk of mental disorders, total internalizing problems and total externalizing problems, according to the child behaviour checklist (CBCL) in the atopic dermatitis group (GDA) and the healthy siblings group (HSG). Pearson’s χ2 test with Yates correction
Regarding CBCL syndromes in the ADG, “Sleep Problems”, “Thought Problems” and “Anxiety/Depression” were the most frequent ones. In the HSG, the most frequent syndromes were “Rule-Breaking Behaviour”, “Thought Problems” and “Aggressive Behaviour” (Table 1).
Table 1
Frequency of syndromes classified as clinical according to the Child Behaviour Checklist (CBCL) in the Atopic Dermatitis Group (ADG) and the Healthy Siblings Group (HSG)
| Syndromes in CBCL | ADG n (%) | HSG n (%) | P-value |
|---|---|---|---|
| Emotional Reactivity | 6 (14.0)1 | 1 (6.3)4 | 0.668 |
| Anxiety/Depression | 25 (25.0)2 | 9 (18.0)5 | 0.607 |
| Isolation | 16 (16.0)2 | 5 (10.0)5 | 0.607 |
| Somatic Complaints | 16 (16.0)2 | 2 (4.0)5 | 0.038 |
| Sleep Problems | 26 (60.5)1 | 2 (12.5)4 | < 0.018 |
| Attention Problems | 20 (20.0)2 | 5 (10.0)5 | 0.297 |
| Aggressive Behaviour | 20 (20.0)2 | 10 (20.0)5 | 0.627 |
| Social Problems | 18 (31.6)3 | 6 (17.6)6 | 0.197 |
| Thought Problems | 28 (49.1)3 | 7 (20.6)6 | 0.017 |
| Rule-Breaking Behaviour | 11 (19.3)3 | 9 (26.5)6 | 0.448 |
Comparing the groups, except for “Rule-Breaking Behaviour”, there was a higher frequency in the ADG for all CBCL syndromes, when compared to the HSG, especially for “Somatic Complaints”, “Sleep Problems” and “Thought Problems” (Table 1). The risk of “Sleep Problems” was twice as high in the ADG participants as in the SG (RR = 2.86; 95% CI: 1.18–6.92).
Answers to CBCL’s open-ended question “What are your biggest concerns regarding your child?” were categorized and presented in Table 2. With regards to parental concerns of the ADG, symptoms related to the disease, such as pruritus, appearance of lesions, chronicity and treatment expenses, were the most frequent mentions. The second concern was related to socialization/bullying problems (including physical and verbal abuse and social exclusion). Lastly, parents mentioned concern related to low academic performance. Regarding the HSG, the main concerns were related to low academic performance, followed by minor illnesses, and socialization/bullying problems.
Table 2
Frequency of responses to the open-ended question of the child behaviour checklist (CBCL) “What are your biggest concerns regarding your child?”, in the atopic dermatitis group (ADG) and the healthy siblings group (HSG)
| CBCL concerns | ADG n (%) | HSG n (%) | P-value |
|---|---|---|---|
| Symptoms of AD (ADG)/Minor Illness (HSG) | 46 (46.0)1 | 5 (10.0)2 | < 0.0013 |
| Socialization/Bullying | 33 (33.0)1 | 2 (4.0)2 | < 0.0014 |
| Academic Performance | 15 (15.0)1 | 12 (24.0)2 | 0.173 |
Discussion
The risk of MD was higher in children and adolescents with AD (63.0%) than in their healthy siblings (36.0%), and higher than the estimates for the general Brazilian population (24.6%) [12]. These data are corroborated in the literature, suggesting that AD may contribute to the development of MD [1, 5–7]. These results are similar to those found by Catal et al. [6] who measured through the Early Childhood Inventory-4 (ECI-4) that 69% of the children with AD had at least one psychiatric diagnosis.
Amongst the syndromes evaluated, “Sleep Problems” was the most observed syndrome (60.5%) in the ADG. Similar results were found in other studies, such as the research by Ridolo et al. [13] which evaluated sleep-related problems in 62.3% of the children with AD through the Pittsburgh Sleep Quality Index (PSQI). The frequency observed in this study is similar to that noted in the study by Chamlin et al. [14] who assessed the presence of sleep disorders in 60% of the paediatric patients with AD, and Fishbein et al. [15], who identified sleep problems in 60% of the children and adolescents with AD. These two results were obtained by means of the Children’s Dermatology Life Quality Index (CDLQI).
The second most frequent syndrome was “Thought Problems”, observed in 49.1% of the ADG. According to parents, their children have presented persistent thoughts due to their concern about the disease and its effects. Most of them have stated that their children frequently manipulate parts of their body and remove scaling skin or eczema. The high frequency of the syndrome “Thought Problems” in the paediatric population with AD was found in the literature by a study that used CBCL to evaluate 25 children diagnosed with AD and 25 controls. The children in the group with AD were more concerned and rigid in their thoughts in comparison to the controls (32.0% vs. 4.0%) [16]. In the present study, it was found that the complexity of details in the daily management of the disease as well as the lack of emotional strategies of the child and/or adolescent to deal with AD lead to the repetition of thoughts and acts that characterize this syndrome.
The third most frequent syndrome in the ADG was “Anxiety/Depression”, observed in 25% of the cases. Similar results were found in a study by Slattery et al. [17], who diagnosed Anxiety Disorder in 26% of the paediatric population with AD through the Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime version (K-SADS-PL). In a study by Catal et al. [6], who evaluated 80 children with AD, the frequency of anxiety was 13%. The divergence of these studies may result from the use of different instruments (CBCL, K-SADS-PL and ECI-4), as well as the different age groups evaluated (1 year and 6 months – 14 years, 13–17 years, and 3–5 years, respectively). Another difference among the studies is that this study used risk criteria for MD and the two studies used diagnostic criteria.
In the present research, 33% of the ADG cases reported that children and/or adolescents suffered physical/verbal violence (bullying). In 31.6% of the cases, “Social Problems” were observed, and in 16%, signs of “Isolation” were observed. These signs are mainly identified by statements, in which they affirm that they prefer being alone rather than with others, being reserved, and keeping their thoughts and feelings to themselves. These results are in accordance with studies that affirm that children and adolescents with AD suffer social isolation and peer rejection [17–19]. Thus, conviviality and management of AD may interfere with the emotional and social development of the children and/or adolescents and their family members.
Siblings of children and adolescents with chronic diseases constitute a population at risk for MD. However, since there are no studies on MD in siblings of children and adolescents with AD so far, the literature used in this study was based on siblings of children and adolescents with other chronic diseases [20–23]. In the present study, the risk of MD was found in 36.0% in the HSG. A similar frequency was described in a study by Besier et al. [21], in which 30.5% of the healthy siblings of children with cancer, cystic fibrosis and congenital heart disease presented emotional problems. Williams et al. [9] found that siblings of children with chronic diseases are twice or three times more likely to present emotional problems than the general population. This situation can be explained by the conflict that these children feel concerning their sibling’s illness, such as fear (of the illness), jealousy, and rage (due to the special attention given to the ill child by the parents). In this group, the syndrome “Rule-Breaking Behaviour” was the most frequent one (26.5%), being characterized by behaviours such as breaking rules, lying, and not feeling guilty after showing inappropriate behaviour. Probably because they are in development, healthy siblings may not understand the special needs of the ill sibling and present inappropriate and/or exaggerated behaviours.
Comparing the ADG and the HSG, the syndrome that presented the highest differences were: “Sleep Problems” (60.5% vs. 12.5%, p < 0.01), “Thought Problems” (49.1% vs. 20.6%, p = 0.01), and “Somatic Complaints” (16.0% vs. 4.0%, p = 0.03). Thus, the analysis of the results shows that the chronic and relapsed nature of the skin disease affects the patient. Besides, it enhances data on the risk of MD in healthy siblings of children and adolescents with AD. Such result has not been published in the literature yet.
Children and adolescents – healthy or with chronic diseases – have the same needs during their development. Nonetheless, meeting the needs that are characteristic of each stage of child development and, simultaneously, dealing with stressful factors caused by a chronic disease is more difficult for the ill child [23]. Symptoms and conviviality with the disease may change and even aggravate the mental development of the child and adolescent, as well as interfere in their interaction with the environment.
The present study presented limitations; for instance, data on the participants’ behaviour were obtained through a single source of information, in this case, the main parent or guardian who was accompanying the patient during the outpatient visit. It is also necessary to consider the lack of evaluation of the causality of associations, considering the cross-sectional nature of this study. Longitudinal studies may verify the persistence of symptoms, as well as the conditions associated with their attenuation or intensification over time. The use of screening tools by healthcare teams is also recommended to prevent mental healthcare problems.
Conclusions
Children and adolescents with AD present a high risk of MD, greater than the one expected for the general paediatric population. The healthy siblings of these children and adolescents also exhibit impairment in their mental health. However, the frequency of risk factors is lower when compared to their siblings with AD. Nevertheless, this group presents a higher risk than the one expected for the general paediatric population.